Table of Contents
Overview
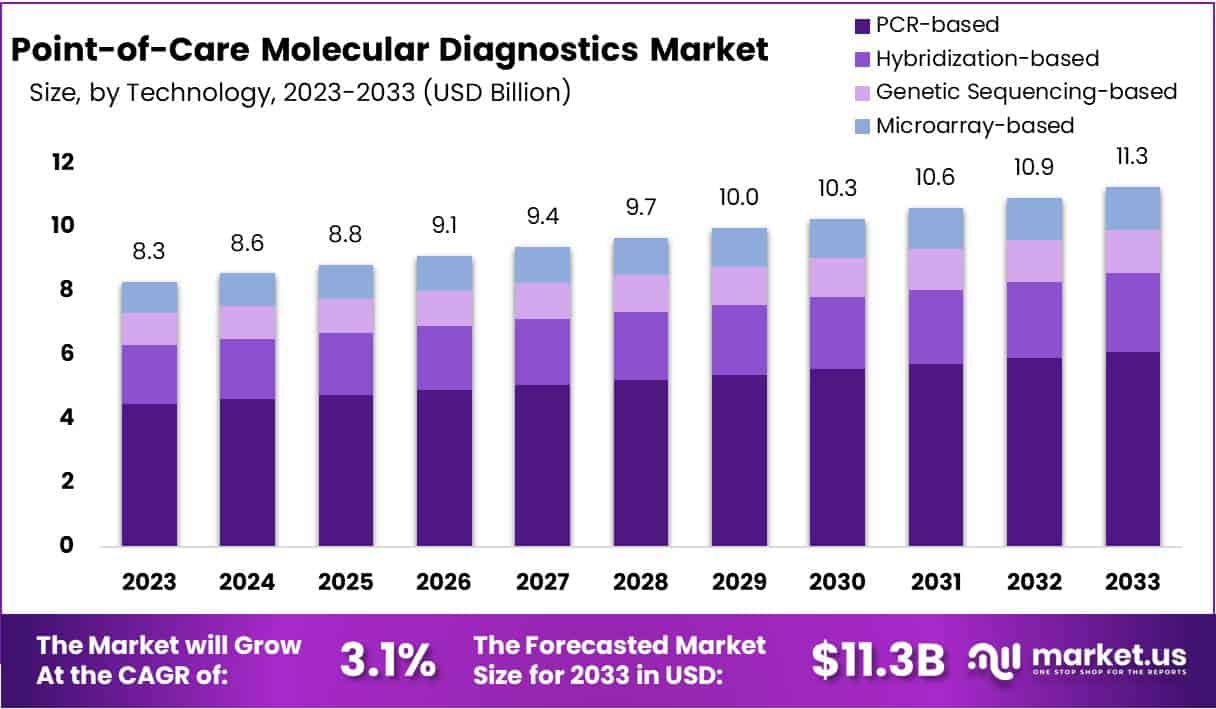
New York, NY – July 11, 2025: The Global Point-of-Care (POC) Molecular Diagnostics Market is projected to grow from USD 8.3 billion in 2023 to USD 11.3 billion by 2033, expanding at a CAGR of 3.1% during the forecast period. This growth is driven by increasing demand for decentralized diagnostic tools, particularly in settings with limited access to centralized laboratories. The ability to deliver accurate and timely results near the patient has become essential in healthcare. Rising pressure to enhance disease surveillance and reduce turnaround times is accelerating the shift toward POC molecular solutions across clinical environments.
A key growth driver is the global rise in infectious and chronic diseases. Conditions such as tuberculosis, influenza, HIV, and cardiovascular disorders continue to place significant pressure on healthcare systems. The World Health Organization (WHO) has identified rapid molecular tests for infectious diseases and drug resistance as a top global priority. These tools help detect pathogens early and ensure timely treatment. Similarly, for chronic illnesses like diabetes, regular and efficient monitoring at the point-of-care supports ongoing management and intervention strategies.
Technological advancement in miniaturized diagnostic platforms is also supporting market expansion. Innovations in microfluidics, lab-on-a-chip designs, and multiplex PCR enable fast and precise testing from a single sample. These platforms are compact, user-friendly, and require minimal infrastructure, making them ideal for decentralized settings. Such progress ensures that molecular testing can be conducted not only in hospitals but also in clinics, mobile units, and rural areas with limited resources.
Government and multilateral investment play a crucial role in making POC diagnostics more accessible. Public institutions and global health agencies are allocating funds to promote the development and distribution of low-cost, high-impact diagnostics. The WHO has recommended tools like the Truenat TB assay for national use, and organizations like the Foundation for Innovative New Diagnostics (FIND) have committed over USD 21 million to support similar platforms. These efforts aim to improve diagnostic coverage in low- and middle-income countries and align with broader goals of healthcare equity and universal health coverage.
Lastly, changing models of care are creating more demand for POC diagnostics. Health systems are moving away from centralized approaches and integrating diagnostics into community health centers, primary care units, and emergency rooms. This shift is driven by the need to reduce delays and improve patient outcomes through rapid clinical decisions. In parallel, awareness about the benefits of early and accurate diagnosis is growing among both patients and providers, further supporting adoption of molecular testing at the point of care.
Key Takeaways
- The global market is anticipated to expand from USD 8.3 billion in 2023 to USD 11.3 billion by 2033, growing at a 3.1% CAGR.
- PCR-based diagnostics captured 54% market share in 2023, widely preferred for their accuracy, speed, and reliability in identifying infectious agents.
- Infectious diseases emerged as the dominant application, representing over 30% of the market, owing to rising global demand for quick and precise diagnostic solutions.
- Over-The-Counter (OTC) diagnostics held 51.7% market share, fueled by increased consumer preference for convenient, accessible testing options outside clinical settings.
- Decentralized labs accounted for more than 33% of end-use share, reflecting a growing trend toward immediate and location-flexible diagnostic services.
- North America led with a 38% market share in 2023, driven by strong healthcare infrastructure and supportive government regulatory environments.
Emerging Trends
- AI and Machine Learning Integration: Artificial intelligence (AI) and machine learning (ML) are being added to POC molecular diagnostics. These tools, especially convolutional neural networks (CNNs), help process test results faster and with greater accuracy. They also remove the need for expert technicians to interpret data. As a result, the overall turnaround time is reduced. This makes real-time diagnosis possible even in non-specialized settings. AI-based POC devices are increasingly used for conditions like COVID-19, HIV, and flu. They improve reliability while reducing human error. These smart systems are also being designed to learn from large datasets, improving test quality over time.
- CRISPR-Based Testing at the Point of Care: CRISPR technology is transforming molecular diagnostics. It is now being applied to point-of-care (POC) testing. CRISPR-based platforms can detect infectious diseases such as tuberculosis, malaria, Zika virus, and HPV. Some new devices are even able to identify certain cancer biomarkers. These tests are fast, affordable, and accurate. They work by targeting specific DNA or RNA sequences. With minimal equipment, results can be obtained in under an hour. The simplicity and precision of CRISPR make it ideal for use in low-resource areas. Researchers are also working on expanding its use for broader disease detection at the point of care.
- Multiplexed Testing Capabilities: Multiplex testing is a growing trend in POC diagnostics. It allows the detection of multiple pathogens or biomarkers from one sample. This improves efficiency and saves time for both patients and healthcare providers. For example, a single test can now screen for flu, COVID-19, and RSV at once. This capability lowers testing costs and speeds up treatment decisions. It also reduces the number of tests needed per patient. Multiplex assays are especially useful during disease outbreaks. They are being adopted in clinics, emergency rooms, and even for at-home testing. This makes diagnostics faster and more accessible than ever.
- Microfluidics and Lab-on-Chip Miniaturization: Lab-on-a-chip technology is making molecular testing smaller and faster. These devices use microfluidics to control small fluid volumes. They can process samples quickly and deliver results in just a few minutes. Some platforms, for example, provide SARS-CoV-2 results in under three minutes. These tools require very little sample material and are easy to carry. Their compact size makes them ideal for mobile health settings. They are also energy efficient and work with minimal training. The push toward miniaturization is helping diagnostics reach people in remote and underserved areas without sacrificing accuracy or speed.
- Portable Platforms for Low-Resource Settings: Portable molecular diagnostic tools are now built for use in remote and low-resource environments. These lightweight devices are often battery-powered and highly efficient. They can detect diseases such as mpox or tuberculosis with high accuracy. Some show over 94% sensitivity and nearly 100% specificity. Because they do not need complex lab infrastructure, these platforms are ideal for field testing. Many also feature easy-to-use interfaces. They work well even in regions with limited electricity or trained personnel. By offering accurate testing at the point of care, these tools help improve public health outcomes in underserved communities.
- Enhanced Sensitivity and Patient Safety: New diagnostic methods are making point-of-care tests more sensitive and safe. Technologies like chemiluminescence and nanoparticle amplification can detect extremely small amounts of disease markers. For instance, cardiac troponin I can now be identified in as little as 15 to 25 minutes. These advanced assays help catch health issues early, improving patient outcomes. High-sensitivity tools are crucial for detecting heart attacks, infections, and cancers. They also reduce false negatives and support faster clinical decisions. As safety standards rise, these innovations ensure patients receive accurate results with minimal risk.
- Interoperability and Data Connectivity: The future of POC diagnostics includes better data integration. Devices are now designed to share data easily with electronic health records (EHRs). This supports faster communication between patients, labs, and healthcare providers. Governments and regulators like the FDA are also pushing for clear guidelines on data sharing. This ensures that patient records remain safe and private. With improved connectivity, test results can be tracked in real time. This also helps in managing outbreaks and improving public health monitoring. Interoperable systems make POC diagnostics more efficient, accurate, and connected to the broader healthcare system.
Use Cases
- Infectious Disease Diagnosis in Field Settings: Point-of-care (POC) PCR platforms help in fast and accurate diagnosis of infectious diseases. For example, in a Monkeypox (mpox) study, 164 samples were tested using a portable POC PCR tool. Among them, 51 were mpox-positive. The test achieved 96.1% sensitivity and 100% specificity. For tuberculosis (TB), the GeneXpert MTB/RIF platform detects TB DNA and rifampicin resistance in less than 90 minutes. It delivers 89–92% sensitivity and 99% specificity. In India, the use of Molbio’s TrueNat platform improved TB detection rates by about 30% after implementation. These technologies are proving useful in resource-limited and outbreak-prone settings.
- Urine-Based TB Detection in HIV Patients: POC tests also benefit patients with HIV, who are at higher risk for TB. The Fujifilm SILVAMP TB LAM test is one such tool. It uses urine samples to detect TB quickly and accurately. Among around 1,595 HIV-positive patient samples, it achieved 71% sensitivity and 91% specificity. In hospitalized HIV-positive patients, the test diagnosed nearly 89% of TB cases within 24 hours. This rapid diagnosis supports earlier treatment decisions. It also reduces the risk of disease progression or death. The test is especially valuable in low-resource settings where conventional TB diagnosis takes longer.
- Rapid COVID-19 Testing at Clinics: During the COVID-19 pandemic, POC molecular diagnostics played a key role. Tools like the Cepheid GeneXpert and Abbott ID NOW were used widely in clinics. These systems delivered reliable COVID-19 results in just 5 to 60 minutes. This allowed healthcare workers to isolate patients quickly and begin treatment. The fast results also supported testing in emergency departments and rural areas. Rapid testing reduced lab burden and improved access. These platforms helped manage the spread of infection and supported faster clinical decisions during critical times.
- High-Sensitivity Cardiac Marker Detection: Advanced POC tools are now capable of detecting heart conditions at early stages. The chemiluminescence vertical flow assay (VFA) detects cardiac troponin I at very low levels—just 0.16 pg/mL—in 25 minutes. The variation in results is less than 15%, showing high reliability. Another paper-based nanoparticle VFA detects troponin I at 0.2 pg/mL in 15 minutes, with a coefficient of variation (CV) under 7%. These tools match the accuracy of central lab tests. They help clinicians quickly assess patients with chest pain, especially in emergency settings.
- Pharmacogenomics at the Bedside: Point-of-care genetic testing is improving personalized medicine. The CYP2C19 genetic test (RAPID GENE) is used at the bedside. It identifies how patients metabolize clopidogrel, a common antiplatelet drug. This test supports quick decisions during acute coronary interventions. For patients with genetic variants, the test helps guide safer and more effective therapy. Results are available quickly, allowing immediate clinical action. This reduces complications and improves outcomes. Bedside pharmacogenomics is becoming a valuable part of personalized care in cardiology and emergency medicine.
Conclusion
In conclusion, point-of-care molecular diagnostics are becoming an essential part of modern healthcare. They offer fast, accurate, and reliable results near the patient, supporting quicker clinical decisions and better outcomes. These tools are especially helpful in remote areas and during health emergencies, where time and access to labs are limited. Innovations such as CRISPR, microfluidics, and AI are making tests smaller, smarter, and more accessible. As more health systems move toward decentralized care, the demand for point-of-care diagnostics is expected to grow further. With support from global health agencies and continued technological progress, these solutions are set to play a major role in improving healthcare delivery worldwide.
Discuss your needs with our analyst
Please share your requirements with more details so our analyst can check if they can solve your problem(s)



