Table of Contents
Introduction
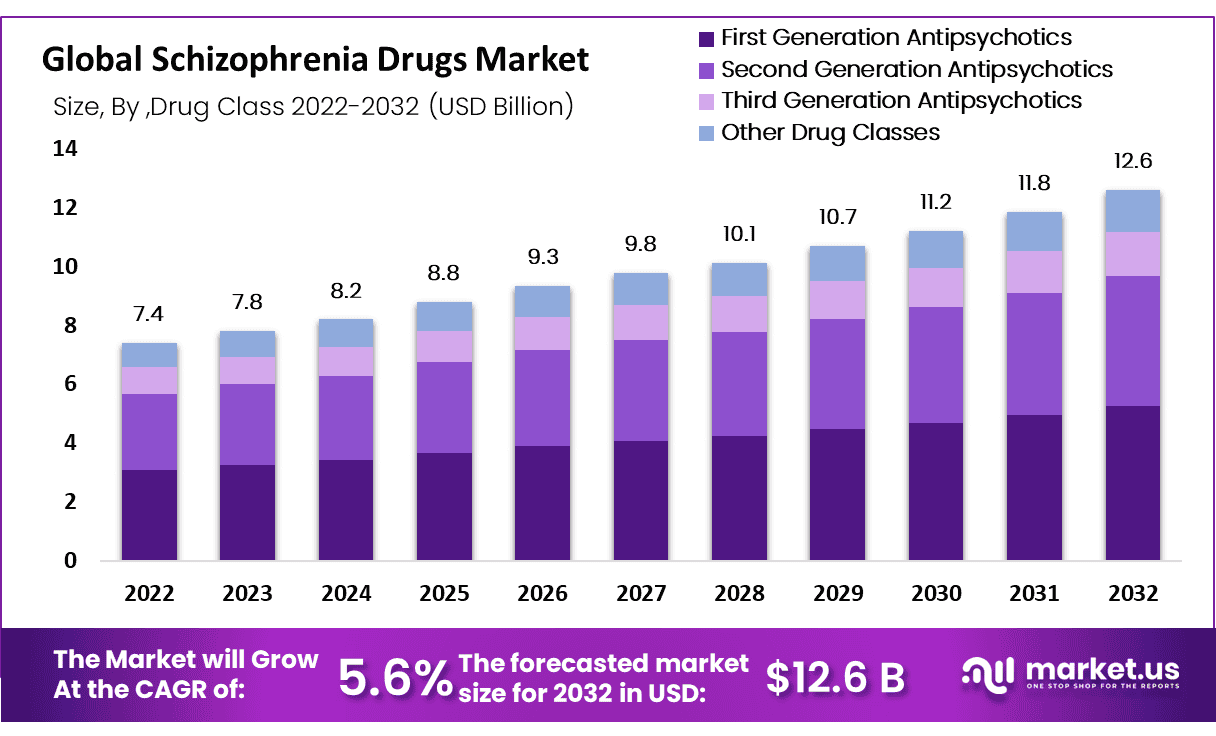
The global schizophrenia drugs market is poised to grow from USD 7.4 billion in 2022 to USD 12.6 billion by 2032, exhibiting a CAGR of 5.6% from 2023 to 2032. Schizophrenia, a severe mental disorder, typically emerges in late adolescence or early adulthood, marked by symptoms such as delusions, hallucinations, disordered thinking, and social withdrawal. The demand for antipsychotic medications is expected to surge due to increasing schizophrenia prevalence, an aging population, and enhanced mental health awareness campaigns, which collectively contribute to market growth.
The growth of the schizophrenia drugs market is driven by several key factors. One primary driver is the increasing understanding of the genetic basis of schizophrenia. Research has mapped the genetic landscape of schizophrenia, revealing that variations in genes such as C4 are linked to the disorder. This genetic insight is essential for developing targeted therapies that can effectively address the biological mechanisms of schizophrenia, potentially leading to more effective treatments. This has sparked significant interest and investment in the development of new schizophrenia medications.
Advancements in clinical trial methodologies are also contributing to market growth. The FDA has identified ways to streamline clinical trials for schizophrenia drugs, making them more efficient and less costly. By shortening the duration of trials and simplifying the assessment tools used to measure disease severity, researchers can reduce patient dropout rates and accelerate the development of new treatments. These improvements are critical in bringing new, effective treatments to market more quickly and efficiently, addressing the unmet needs of patients with schizophrenia.
Additionally, the recognition of schizophrenia as a chronic and severe mental disorder that requires long-term management has led to increased investment in drug development. Effective treatments can help individuals with schizophrenia maintain employment, achieve independence, and improve their overall quality of life. This ongoing need for comprehensive treatment options fuels the demand for new and improved medications. Consequently, pharmaceutical companies are focusing on innovative solutions to meet this growing demand and improve patient outcomes.
Recent developments in the schizophrenia drugs market highlight significant progress and new collaborations aimed at improving treatment options and accessibility. In September 2023, a collaboration was formed to develop and commercialize biosimilar versions of levocetirizine, which could make effective medication more affordable in developing countries. This partnership aims to reduce costs compared to brand-name drugs, enhancing accessibility for patients in need. Such collaborations are pivotal in ensuring that effective treatments are available to a broader patient population.
In October 2023, another collaboration was announced to develop ALX-370, an antihistamine for treating allergic rhinitis and chronic idiopathic urticaria. This partnership leverages expertise in drug delivery platform innovation to enhance the development process and maximize the potential of this groundbreaking antihistamine. These collaborative efforts underscore the industry’s commitment to innovation and patient care, ensuring that new treatments are not only effective but also accessible to those who need them most.
Key Takeaways
- Market Size: The human antihistamine drugs market is projected to reach approximately USD 706.2 million by 2033, significantly up from USD 274.8 million in 2023.
- Market Growth: Market growth is anticipated to occur at a Compound Annual Growth Rate (CAGR) of 9.9% from 2024 to 2033.
- Regional Analysis: In 2023, North America established itself as a key player in the Human Antihistamine Drug Market, achieving a leading position with a significant 37.2% market share and a market value of USD 102.2 million for the year.
- Type Analysis: OTC (Over-the-Counter) medications took the lead in 2023 by garnering more than 60.7% market share.
- End User Analysis: In 2023, the Hospitals segment emerged as the frontrunner in the Human Antihistamine Drug Market, securing a commanding position with over 46.8% of the market share.
- Indication Analysis: In 2023, allergy drugs dominated the human antihistamine drug market, capturing 62.7% of the market share. This indicates a strong consumer preference for antihistamine medications to address allergic conditions and adverse reactions to certain substances.
- Drug Type Analysis: In 2023, Second-Generation Antihistamines dominated the Human Antihistamine Drug Market, capturing over 62.7% of the market share. This reflects strong consumer demand and healthcare provider preferences for advanced antihistamines.
- Genetic Insights: Research has mapped the genetic landscape of schizophrenia, identifying variations in genes such as C4 that are linked to the disorder. This genetic understanding is crucial for developing targeted therapies that address the biological mechanisms of schizophrenia.
- Improved Clinical Trials: The U.S. Food and Drug Administration (FDA) has identified ways to streamline clinical trials for schizophrenia drugs, making them more efficient and less costly. By shortening trial durations and simplifying assessment tools, researchers can reduce patient dropout rates and accelerate the development of new treatments.
- Long-term Management: Schizophrenia is recognized as a chronic and severe mental disorder that requires long-term management. Effective treatments are essential for helping individuals maintain employment, achieve independence, and improve their quality of life.
Schizophrenia Drugs Statistics
- Around 25% of acute schizophrenia patients do not benefit from first-generation antipsychotics like haloperidol.
- Clozapine shows effectiveness in 30-60% of cases unresponsive to other antipsychotics, prescribed to 5-10% of patients.
- Regular monitoring is required with clozapine due to potential side effects, despite its effectiveness in resistant cases.
- Treatment-resistant schizophrenia affects about 20% of patients, with up to 34% showing resistance to multiple therapies.
- Around 60% of patients with treatment-resistant schizophrenia do not improve with clozapine.
- Lurasidone reduces relapse risk by 40% over 12 months in schizophrenia patients.
- In clinical trials, quetiapine significantly improved symptoms in 70% of acute schizophrenia patients.
- Combining antipsychotic medications is part of 10-20% of treatment plans to increase efficacy and manage symptoms better.
- Newer antipsychotics are prescribed to 55.2% of patients, while older versions are used in 44.8% of cases.
- Lurasidone and Quetiapine XR show comparable efficacy in preventing schizophrenia relapses over 12 months.
- About 18% of patients on long-acting injectable antipsychotics relapse within one year.
- A 5% incidence of asymptomatic bradycardia is associated with amisulpride in treating schizophrenia.
- Schizophrenia impacts roughly 20 million people globally, with a prevalence of 0.33% to 0.75% internationally.
- In the U.S., schizophrenia affects about 0.25% to 0.64% of the population.
- Schizophrenia is among the top 15 disabilities globally, significantly reducing life expectancy.
- On average, individuals with schizophrenia lose 28.5 years due to premature mortality.
- Suicide accounts for 5% to 6% of deaths among those with schizophrenia.
- Nearly 50% of those with schizophrenia also experience co-occurring mental or behavioral disorders.
- Regular cigarette smoking is prevalent in about half of the individuals with schizophrenia.
- Annually, the total economic burden of schizophrenia reaches nearly $63 million.
- The cost of treating schizophrenia is six times higher than that for heart disease.
- Only about 31% of individuals with schizophrenia have access to healthcare services.
- Less than one-third of those with schizophrenia are receiving treatment.
- Over two-thirds of individuals with psychosis lack access to specialized mental health care.
- Half of the people with schizophrenia have struggled with substance abuse.
- In the U.S., 26% of those with schizophrenia use street drugs, and 53% use cannabis.
- Having a first-degree relative with schizophrenia increases one’s risk by 10%.
- Environmental factors like birth complications and malnutrition can elevate the risk of schizophrenia.
- The typical onset of schizophrenia occurs from the late teens to the early thirties, but can appear as late as age 70.
- In the UK, around 220,000 people receive treatment for schizophrenia through the NHS.
- Only 31.3% of individuals with psychosis in the UK receive care from mental health specialists.
- Mental illness imposes a significant economic burden, costing the UK economy about £77 billion annually, or roughly 4% of its GDP.
- The life expectancy for those with schizophrenia is reduced by an average of 28.5 years compared to the general population.
Emerging Trends
- Rise in Personalized Medicine: Personalized medicine for schizophrenia involves the use of genetic testing to determine how a patient will respond to specific drugs. This approach aims to enhance drug efficacy and minimize adverse effects. Genetic markers can predict patient responses to antipsychotic medications, allowing for more tailored treatments. Personalized treatment plans can include adjustments in drug types and dosages based on individual genetic profiles.
- Development of Novel Antipsychotics: The development of novel antipsychotics is focused on reducing side effects such as weight gain, diabetes, and cardiovascular issues associated with traditional antipsychotics. New drugs, like lumateperone and cariprazine, target both positive symptoms (hallucinations and delusions) and negative symptoms (social withdrawal and apathy) of schizophrenia. These novel antipsychotics also aim to improve cognitive function and overall patient compliance.
- Increased Focus on Long-Acting Injectables: Long-acting injectables (LAIs) provide a sustained release of medication, improving adherence and reducing the risk of relapse. LAIs can be administered every two weeks to three months, offering a convenient alternative to daily oral medications. Drugs like paliperidone palmitate and aripiprazole lauroxil are examples of LAIs that have shown efficacy in maintaining symptom control and reducing hospitalization rates.
- Advancements in Digital Health Technologies: Digital health technologies are revolutionizing the management of schizophrenia. Mobile apps and wearable devices can track medication adherence, monitor symptoms, and provide real-time feedback to healthcare providers. These technologies enable remote patient monitoring, allowing for timely interventions and personalized care adjustments. For example, apps like Wellpath monitor patient behavior and adherence to treatment plans, enhancing overall treatment effectiveness.
- Expansion of Telehealth Services: Telehealth services have expanded significantly, offering greater access to mental health care, especially in rural and underserved areas. Telepsychiatry allows patients to receive consultations, therapy sessions, and medication management remotely. This expansion has been accelerated by the COVID-19 pandemic, highlighting the need for accessible mental health services. Studies have shown that telehealth is effective in maintaining patient engagement and treatment continuity.
- Increased Research in Glutamate Receptor Modulators: Glutamate receptor modulators are being explored as potential treatments for schizophrenia, targeting the glutamate system rather than the dopamine system. Drugs like bitopertin and glycine have shown promise in clinical trials for improving negative symptoms and cognitive deficits. This research represents a shift from traditional antipsychotics, offering new hope for patients who do not respond well to existing treatments.
Use Cases
- Management of Acute Psychotic Episodes: Schizophrenia medications, especially antipsychotics, are essential for handling acute psychotic episodes. They help alleviate symptoms such as hallucinations and delusions, providing rapid relief during severe episodes. These drugs stabilize patients quickly, allowing them to regain a sense of reality and function more effectively in daily life. Proper management of acute episodes is crucial to prevent potential harm to the patient and others.
- Long-term Maintenance Therapy: For preventing relapses, long-term use of antipsychotic medications is critical. Second-generation antipsychotics are commonly prescribed due to their effectiveness and relatively mild side effects. These medications help maintain stability, reducing the risk of recurring episodes and improving patients’ quality of life. Consistent long-term therapy is essential for managing symptoms over time and reducing the need for hospitalization.
- Addressing Negative Symptoms: Schizophrenia medications are used to manage negative symptoms, such as lack of motivation, social withdrawal, and impaired functioning. These symptoms significantly affect daily life and social interactions. Effective treatment of these symptoms is vital for helping patients engage in social and occupational activities, enhancing overall life satisfaction, and reducing the burden on caregivers.
- Enhancing Cognitive Function: Some antipsychotic drugs aim to improve cognitive functions, addressing issues like attention and memory deficits associated with schizophrenia. These medications can help patients perform better in cognitive tasks and daily activities. Enhancing cognitive function is crucial for patients to live independently, pursue education and employment opportunities, and manage daily responsibilities more effectively.
- Early Intervention: Early treatment with antipsychotic medications can greatly improve the prognosis of schizophrenia. By mitigating the severity of symptoms and improving long-term outcomes, early intervention helps in better managing the disorder. Prompt treatment can prevent disease progression, reduce the duration of untreated psychosis, and lead to better recovery outcomes.
- Combating Substance Abuse-Related Schizophrenia: Addressing substance abuse, particularly cannabis use disorder, is crucial as it is a modifiable risk factor for schizophrenia. Integrating substance abuse treatment with psychiatric care can help reduce the incidence of schizophrenia, especially among young men. Comprehensive treatment programs that address both substance abuse and schizophrenia can decrease the overall burden of the disorder.
- Support in Hospital Settings: Hospital pharmacies are crucial in providing schizophrenia medications to both inpatients and outpatients. They ensure a continuous supply of medications and adherence to prescribed therapies, which is vital for managing both acute and chronic phases of the disorder. By maintaining a reliable supply chain and offering expert pharmaceutical care, hospital pharmacies play a significant role in the effective management and recovery of schizophrenia patients.
Conclusion
The schizophrenia drugs market continues to evolve, driven by advances in treatment options and a growing understanding of the disease. Ongoing research and development efforts, particularly in second and third-generation antipsychotics, are enhancing the efficacy and safety profiles of these medications. Early intervention and long-term maintenance therapies are critical in managing the disease, improving patient outcomes, and reducing healthcare costs. Furthermore, integrating telehealth and innovative clinical trial designs are streamlining the development and distribution of new treatments. The market’s growth is supported by robust healthcare infrastructure and regulatory frameworks, ensuring that new, effective medications are available to those in need, ultimately improving the quality of life for patients with schizophrenia.
Discuss your needs with our analyst
Please share your requirements with more details so our analyst can check if they can solve your problem(s)



