Table of Contents
Overview
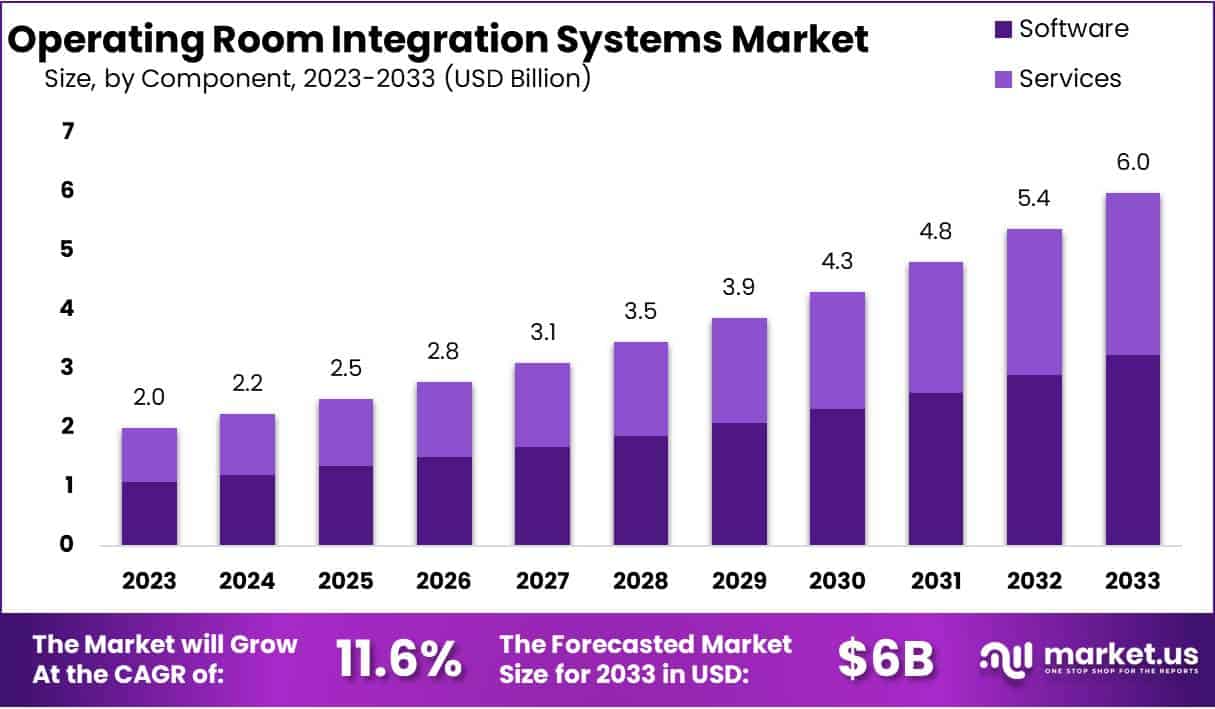
New York, NY – June 24, 2025: The Global Operating Room (OR) Integration Systems Market is projected to reach USD 6 billion by 2033, up from USD 2 billion in 2023. This growth reflects a strong compound annual growth rate (CAGR) of 11.6% during 2024–2033. The rise in market value is mainly driven by increasing demand for minimally invasive surgeries (MIS), the need to enhance workflow efficiency, digital health adoption, and supportive government policies.
Minimally invasive surgeries are growing rapidly due to their benefits, including faster recovery and reduced trauma. However, these procedures require high-definition imaging, real-time data systems, and seamless navigation tools. As a result, hospitals are adopting hybrid ORs equipped with advanced integration systems. These setups improve surgical precision by unifying video, audio, and imaging data on one platform. They also support the increasing use of robotic and image-guided surgeries in complex medical procedures.
Operational efficiency and patient safety are major concerns in surgical environments. OR integration systems help reduce human errors and communication delays by streamlining data flow. These systems integrate surgical video feeds, patient records, and device controls, minimizing disruptions. Studies highlight that poor perioperative communication contributes to adverse outcomes. By reducing this risk, integrated systems improve care quality while also supporting faster decision-making during surgeries.
Government and global policy frameworks are also accelerating adoption. The World Health Organization’s Global Strategy on Digital Health 2020–2025 promotes the use of technologies like the Internet of Things (IoT), AI, and cloud platforms for healthcare delivery. In 2023, WHO and the G20 launched the Global Initiative on Digital Health to strengthen governance and investment in digital infrastructure. These initiatives directly encourage OR digital integration by promoting interoperability and data sharing.
At the national level, the European Health Data Space regulation (effective from March 2025) enforces standards for electronic health data exchange across clinical settings. India’s Ayushman Bharat Digital Mission is building a nationwide digital health infrastructure, enabling real-time access to patient records. In the United States, the CMS publishes performance metrics, including OR efficiency scores, pushing hospitals to adopt smart integration tools. Combined with advancements in AI, 4K imaging, and IoT, these policies and technologies create a strong foundation for market expansion.
Key Takeaways
- The operating room integration market is projected to reach USD 6 billion by 2033, growing steadily at a CAGR of 11.6% from 2024.
- Software remains the most dominant component, contributing to 54% of the market due to its role in centralizing and streamlining OR operations.
- Documentation management systems accounted for over 42% of the device type market share in 2023, making them essential for surgical data handling.
- General surgery held a commanding 42% share among applications in 2023, reflecting its frequent use of integrated OR technologies across procedures.
- Hospitals dominated end-user adoption with more than 57% market share in 2023, owing to high surgical volumes and infrastructure readiness.
- The rise in minimally invasive surgeries has become a major driver, reducing hospital procedure time by 30% and increasing OR integration demand.
- The integration of artificial intelligence and machine learning is opening new possibilities for surgical precision, workflow automation, and clinical decision-making.
- High initial costs, averaging USD 1 million per integrated OR, continue to act as a significant barrier to broader market adoption.
- With increasing digitalization, concerns around data privacy have intensified, prompting stronger cybersecurity measures in integrated operating environments.
- North America led the market with over 38% share in 2023, supported by advanced healthcare systems and high investments in surgical innovation.
Emerging Trends
- Enhanced Visualization and Imaging: Modern ORs now use high-definition (HD), 4K, and 3D imaging systems to support surgical accuracy. These systems offer surgeons a clearer and more detailed view of internal structures. They are especially helpful during minimally invasive or complex surgeries. Hybrid operating rooms (ORs) are also gaining popularity. These rooms come with built-in imaging devices like CT scans, MRIs, and fixed C-arms. Surgeons use them in cardiovascular, orthopedic, and neurosurgery procedures. The real-time imaging improves decision-making during surgery. It reduces the need to shift patients between rooms. This leads to better surgical outcomes and faster recovery times for patients. It also supports a safer and more efficient workflow.
- AI and Machine Learning Integration: Artificial intelligence (AI) is playing a growing role in operating room efficiency. Hospitals are using AI-based tools to manage surgical scheduling and predict patient risk. These tools also help reduce errors and optimize workflow in real time. Machine learning can analyze past data and suggest the best course of action during surgery. This improves outcomes and shortens recovery time. AI systems also help streamline inventory, equipment use, and staff coordination. By reducing human error, these technologies increase patient safety. As hospitals aim for higher efficiency and quality care, AI and machine learning are becoming standard in integrated OR systems worldwide.
- Robotic‑Assisted Surgery: The use of robotic-assisted systems like Da Vinci Xi is rising fast. These systems offer high precision with minimal incisions. Patients benefit from shorter hospital stays and quicker recovery. In the UK’s NHS, robot-assisted surgeries doubled from about 35,000 in 2022 to 70,000 in 2024. This reflects a global trend toward technology-assisted surgeries. Robotic systems are now integrated with imaging tools, AI, and workflow software. This allows surgeons to make accurate and safe decisions during procedures. Hospitals are also adopting these systems to reduce human error and improve consistency. The trend shows strong momentum in both developed and emerging healthcare systems.
- Real‑Time Data and Dashboarding: Modern ORs are becoming smarter with real-time data integration. Surgical teams now use dashboards that combine patient vitals, equipment status, and procedural workflow. This helps improve communication and decision-making during surgery. These unified dashboards reduce delays and enhance team coordination. By viewing all relevant data in one place, teams can quickly respond to changes. It also lowers the risk of human error. Real-time monitoring supports better outcomes and efficient use of resources. As hospitals move toward digital transformation, dashboards are becoming standard in integrated OR systems. This ensures a more organized, transparent, and responsive surgical environment.
- IoT for Device and Supply Tracking: The Internet of Things (IoT) is transforming how operating rooms track devices and supplies. Sensors are used to monitor surgical tools, consumables, and equipment in real time. This improves operational efficiency and reduces delays. It also helps avoid supply shortages and ensures timely restocking. OR staff can focus more on patient care instead of managing inventory manually. IoT also supports equipment maintenance by predicting failures before they occur. With this data, hospitals can reduce downtime and prevent cancellations. The use of IoT leads to cost savings, smoother workflows, and a more reliable surgical environment. It is becoming an essential part of OR integration.
- Cybersecurity and Data Privacy: As ORs become more connected, cybersecurity is now a top concern. Integration systems handle sensitive patient data, medical images, and device controls. This makes them targets for cyberattacks. Hospitals are now including strong security frameworks in their OR systems. Measures such as data encryption, secure access, and regular audits are being used. Cybersecurity also protects the integrity of connected devices and software. Any breach could risk patient safety or delay surgery. To comply with health data laws, hospitals must ensure these systems meet strict privacy standards. Strong cybersecurity is now a key part of every OR integration strategy.
- Flexible OR Layouts: New operating rooms are being designed with flexibility in mind. Modular layouts allow quick adjustments based on the type of surgery. These rooms can easily accommodate new technologies like robotic tools, AI systems, and advanced imaging. Flexible spaces also support hybrid procedures involving multiple specialties. Equipment like surgical lights, monitors, and booms can be reconfigured easily. This reduces setup time and improves team efficiency. It also helps hospitals future-proof their investment as technologies evolve. Such adaptable ORs are in high demand in hospitals aiming for better care and cost-effective operations. Layout flexibility is becoming a core feature in OR planning.
- Remote Collaboration and Tele‑OR: Remote collaboration is changing how surgeries are performed and taught. Surgeons can now guide or assist in procedures remotely using augmented reality (AR) and telecommunication platforms. These Tele-OR systems are especially useful for rural or underserved hospitals. Specialists can join surgeries in real time without traveling. This supports better clinical outcomes and wider access to expert care. The COVID-19 pandemic accelerated the use of these systems. Hospitals now use them for training, mentoring, and live consultations. Tele-OR technology also reduces surgical delays and helps build clinical capacity. It is becoming a standard tool in digitally integrated OR environments.
- Workflow Efficiency and Value-Based Care: OR integration is helping hospitals meet value-based care goals. These systems improve workflow by reducing surgical delays and optimizing schedules. For example, automated tools help start the first surgery on time. They also lower case turnover time and cut cancellation rates. As a result, hospitals can treat more patients with fewer resources. Integrated systems improve coordination among surgical teams, leading to better outcomes. They also help hospitals meet quality and safety targets required by insurers. This aligns with global efforts to improve care while managing costs. Efficiency and patient outcomes are now key metrics in OR integration planning.
- Rise in Minimally Invasive Procedures: Minimally invasive surgeries are becoming more common due to better outcomes and faster recovery. These procedures require advanced tools like real-time imaging and robotic arms. Integrated ORs support such procedures with seamless data flow and imaging access. Patients benefit from smaller incisions, less pain, and shorter hospital stays. This trend is driving hospitals to invest in smarter, more connected surgical environments. Integrated systems ensure that all devices work together efficiently. This improves safety and speeds up the surgery. As demand grows for these procedures, OR integration becomes vital for delivering modern, high-quality surgical care.
Use Cases
- Robotic-Assisted Hysterectomy (NHS, UK): At Chelsea & Westminster Hospital, a robotic-assisted hysterectomy using the Da Vinci Xi system was completed in just 40 minutes. Blood loss was minimal—only around 25 mL. In comparison, traditional hysterectomies took nearly 2 hours and often required overnight hospital stays. Additionally, the robotic method helped reduce costs by approximately €2,300 per case. This sharp increase highlights a growing preference for minimally invasive, precision-led surgical approaches that offer shorter recovery times and better outcomes.
- Robotic Hip Replacement Precision: Robotic systems enable surgeons to plan and execute hip replacements with high accuracy. The process involves 3D mapping, ensuring that implants are aligned with precise angles—similar to using a “spirit level.” This approach limits soft tissue disruption. In fact, only one tendon is cut compared to three in traditional surgeries. As a result, patients often experience faster recovery and reduced post-operative pain. Surgeons gain better control over joint alignment, leading to improved long-term mobility. This method is especially valuable in elderly patients who benefit most from precise reconstruction and minimized trauma during surgery.
- Hybrid Operating Rooms for Cardiovascular Surgery: Hybrid ORs combine advanced imaging with surgical functionality. These rooms are equipped with tools like intraoperative CT scanners and fluoroscopy. Surgeons use real-time 3D images to adjust procedures during vascular or cardiac surgeries. This setup improves the accuracy of repairs, such as stent placements or valve interventions. It also reduces the need for secondary procedures. The integration of imaging and surgery helps treat complex cardiovascular conditions more efficiently. By combining diagnostics and intervention in a single room, hybrid ORs enhance patient safety and reduce total surgical time, especially for high-risk individuals.
- Data-Driven Efficiency in Operating Rooms: Hospitals are now using performance metrics to optimize operating room efficiency. Key indicators include case cancellation rates, turnover times, and first-case start accuracy. Tracking these metrics enables OR teams to identify gaps and improve scheduling. As a result, hospitals report a 10% to 20% increase in room utilization. Staff workload is balanced more effectively, reducing overtime and associated costs. This data-driven strategy helps avoid delays, manage resource allocation, and improve patient flow. In the long term, it also contributes to better surgical outcomes and higher patient satisfaction.
- Remote Surgical Collaboration and Training (Proximie): Proximie’s augmented reality (AR) platform allows surgeons to guide procedures remotely. This tool became essential during the pandemic when trainee exposure dropped by 50%. Within six months, the number of remote surgical sessions increased tenfold. The platform now supports over 20,000 surgical videos. Surgeons can observe, annotate, and provide real-time input from any location. Over 20% of NHS hospitals use this system to support training and collaboration. It helps standardize surgical education, especially in complex or rare procedures, and ensures consistent learning regardless of geographic limitations.
- VR-Based Surgical Training: Virtual reality (VR) is transforming how surgeons are trained. VR simulations provide a risk-free environment to practice complex procedures. Studies show that VR-trained surgeons are better at identifying and correcting errors. Their performance is more consistent compared to those trained with traditional methods. Training sessions are repeatable, customizable, and cost-effective. As a result, new surgeons reach proficiency faster. Hospitals are adopting VR to improve surgical readiness and reduce complications. This method is especially useful for training in high-stakes specialties like neurosurgery, orthopedic surgery, and minimally invasive techniques.
- Surgical Safety Checklists via OR Integration: Operating room systems are now integrating WHO surgical safety checklists directly into their platforms. This integration improves compliance and reduces errors. At one UK hospital, implementing this feature led to a drop in surgical complication rates—from 11% down to 7%. Mortality in emergency laparotomy cases fell from 1.5% to 0.8%. That’s a nearly 38% reduction in perioperative death. Automated checklists help ensure that teams follow every critical safety step. This not only saves lives but also improves the overall culture of safety in high-risk procedures.
Conclusion
In conclusion, the operating room integration market is growing steadily due to rising demand for minimally invasive surgeries, better workflow efficiency, and strong government support. Hospitals are investing in advanced systems to improve surgical accuracy, reduce errors, and enable real-time decision-making. Technologies like AI, robotics, and IoT are becoming key parts of integrated surgical environments. These tools help healthcare teams work faster, safer, and more efficiently. Digital health policies and flexible OR designs are also making adoption easier worldwide. As hospitals focus on delivering high-quality, value-based care, the need for connected and intelligent OR systems will continue to rise. This trend reflects a strong shift toward smarter, patient-centered surgical care.
Discuss your needs with our analyst
Please share your requirements with more details so our analyst can check if they can solve your problem(s)



