Table of Contents
- Introduction
- Editor’s Choice
- Global Nursing Workforce Statistics
- Demographic Profile of Nurses
- Nursing Work Shifts Statistics
- Education Level of Nursing Workforce
- Nursing Salaries Statistics
- Nursing Pay Gap Statistics
- Private Nursing Industry Statistics
- Key Nursing Workers’ Issues and Industry Trends
- Regulations for Nursing Workers
Introduction
According to Nursing Workforce Statistics, The nursing workforce comprises various roles, including Registered Nurses (RNs), Nurse Practitioners (NPs), Licensed Practical Nurses (LPNs), and Nursing Assistants (CNAs), each with distinct responsibilities and educational requirements.
R.N.s, the largest group, typically hold an Associate or Bachelor’s degree and provide comprehensive patient care. N.P.s with advanced degrees offer specialized hospital services.
LPNs and CNAs support patient care under supervision, with LPNs requiring a diploma or certificate and CNAs needing state certification.
The nursing workforce, which exceeds 3 million in the U.S., faces challenges such as shortages and burnout but also benefits from growth in advanced practice roles and diverse career opportunities.
Editor’s Choice
- As of 2021, the number of practicing nurses per 1,000 inhabitants varies significantly across different countries. Finland leads with 18.9 nurses per 1,000 inhabitants.
- The racial and ethnic distribution of registered nurses in the United States shows a significant majority of White nurses comprise 75.4% of the workforce.
- Among inpatient nurses, 17% work shifts of 12 or more hours, and 51% work 12-hour shifts. 12% work 10-hour shifts, 19% work 8-hour shifts, and 1% work less than 8-hour shifts, with another 1% falling into the ‘Other’ category.
- The highest paying countries for nurses, based on average annual salary in USD, reveal various lucrative opportunities across various regions. Luxembourg leads with an average salary of $97,857 per year.
- In 2013, the salary gap between male and female nurses in the U.S. varied significantly by job position, revealing notable disparities. Nurse anesthetists experienced the largest gap, with male nurses earning $17,290 more than their female counterparts.
- In 2023, registered nurses in the United States reported high-stress levels during their work. A significant 56% of respondents indicated experiencing a great deal of stress.
- To increase overall work satisfaction among nursing staff. 68% of respondents indicated that increasing salary, wages, or bonuses would be most effective. Nursing workers perceive various support initiatives as critical to their effectiveness and well-being.
Global Nursing Workforce Statistics
Nurse Density Worldwide – By Country
- As of 2021, the number of practicing nurses per 1,000 inhabitants varies significantly across different countries.
- Finland leads with 18.9 nurses per 1,000 inhabitants, followed closely by Switzerland and Norway, each with 18. Iceland has 15 nurses per 1,000 inhabitants, while Australia and Ireland each have 13.
- Japan, Germany, and the United States report 12.1, 12, and 12 nurses per 1,000 inhabitants, respectively.
- Luxembourg has 11.7, the Netherlands 11.4, Belgium 11.1, and New Zealand 10.9.
- Sweden, Austria, and Slovenia have 10.7, 10.6, and 10.5 nurses per 1,000 inhabitants, respectively. Canada and Denmark have 10.3 and 10.2, respectively.
- France reports 9.7 nurses per 1,000 inhabitants, while the OECD37 average stands at 9.2. The Czech Republic has 9, Korea 8.8, and the United Kingdom 8.7.

Demographic Profile of Nurses
Age Distribution
- The age distribution of the nursing workforce shows notable variations across different Human Development Index (HDI) categories.
- In countries with a Very High HDI, only 0.45% of nurses are under 25 years old. While 23.84% are aged 25-34, 23.16% are 35-44, 21.47% are 45-54, 21.36% are 55-64, and 9.72% are over 64.
- In High HDI countries, the distribution shifts slightly with 2.4% of nurses under 25, 26.36% aged 25-34, 30.03% aged 35-44, 22.7% aged 45-54, 12.97% aged 55-64, and 5.54% over 64.
- Medium HDI countries have 3.68% of nurses under 25, a higher proportion of 37.7% aged 25-34, 28.38% aged 35-44, 17.69% aged 45-54, 10.25% aged 55-64, and only 2.3% over 64.
- In Low HDI countries, 2.98% of the nursing workforce is under 25, 27.05% are aged 25-34, 34.81% are 35-44, 23.79% are 45-54, 8.95% are 55-64, and 2.42% are over 64.

Gender Distribution
- From 2000 to 2018, the gender distribution of nurses worldwide reveals significant regional differences.
- In the African region, 65% of nurses are female and 35% are male.
- The Region of the Americas has the highest percentage of female nurses at 86%, with males comprising 14%.
- In the Eastern Mediterranean region, the distribution is 79% female and 21% male.
- The European region sees 84% of its nursing workforce as female, with 16% being male.
- Similarly, in the Southeast Asia region, 79% of nurses are female and 21% are male.
- Lastly, the Western Pacific region has 81% female nurses and 19% male nurses.

Ethnic and Racial Diversity
Registered Nurses
- The racial and ethnic distribution of registered nurses in the United States shows a significant majority of White nurses comprise 75.4% of the workforce.
- Black or African American nurses make up 23.6%, while Hispanic nurses account for 7.5%.
- Asian nurses represent 3.6% of the nursing population.
- Those identifying as two or more races constitute 1.4%, and American Indian or Alaskan Native nurses make up 0.6% of the total.

Nursing Work Shifts Statistics
Nursing Shift Length – By Care Setting
- The distribution of nursing shift lengths across various care settings. Categorized by age group, highlights significant trends among different age cohorts.
- Among nurses under 25 years old, 8% work in inpatient settings, 7% in emergency departments, 2% in ambulatory care, and 7% in long-term care.
- Nurses aged 25-34 predominantly work in inpatient (34%) and emergency department (36%) settings, with 18% in ambulatory care and 28% in long-term care.
- Those aged 35-44 show a more balanced distribution: 22% in inpatient. 28% in emergency departments, 20% in ambulatory care, and 26% in long-term care.
- Nurses aged 45-54 are primarily found in ambulatory care (25%). With 21% in inpatient settings, 20% in emergency departments, and 19% in long-term care.
- The 55-64 age group has the highest representation in ambulatory care (32%). Followed by inpatient (14%), emergency departments (9%), and long-term care (17%).
- Nurses aged 65 and older are the least represented across all settings, with 1% in inpatient, 4% in ambulatory care, and 2% in long-term care.

Education Level of Nursing Workforce
Education Level of Nursing Assistants in Nursing Homes
- As of 2021, the education level distribution of nursing assistants in U.S. nursing homes reveals a diverse range of educational backgrounds.
- 11% of nursing assistants have less than a high school education.
- The largest group, comprising 43%, are high school graduates.
- Those with some college education but no degree make up 32% of the workforce.
- Meanwhile, 14% of nursing assistants hold an associate’s degree or higher.

Nursing Salaries Statistics
Highest Paying Countries for Nurses
- The highest paying countries for nurses, based on average annual salary in USD, reveal various lucrative opportunities across various regions.
- Luxembourg leads with an average salary of $97,857 per year, followed closely by Switzerland at $93,971 and Denmark at $89,419.
- Nurses in the United Arab Emirates earn an average of $86,759 annually, while those in Australia receive $79,550.
- In the United States, the average salary for nurses is $75,387 per year.
- The Netherlands offers an average annual salary of $73,029, slightly higher than Canada’s $72,729.
- Nurses in Norway earn an average of $71,848 per year, and in Germany, the average annual salary is $69,981.

Nursing Pay Gap Statistics
Salary Gap Between Male and Female Nurses – By Job Position
- In 2013, the salary gap between male and female nurses in the U.S. varied significantly by job position, revealing notable disparities.
- Nurse anesthetists experienced the largest gap, with male nurses earning $17,290 more than their female counterparts.
- Middle management positions saw a gap of $6,918, while senior administrators had a difference of $5,839.
- In advanced practice roles, the salary gap was $5,787, and in education/research positions, it was $5,308.
- Staff nurses faced a gap of $5,277, and those in advanced clinical roles had a gap of $4,328.

Private Nursing Industry Statistics
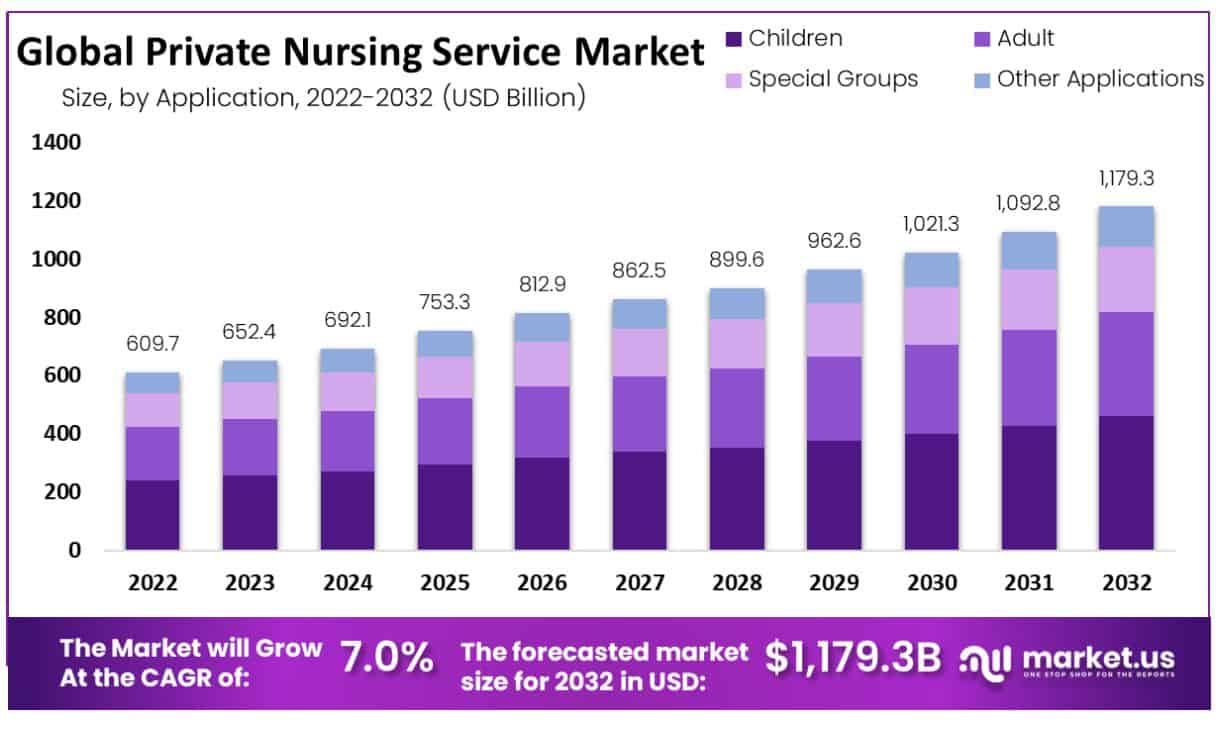
Global Private Nursing Services Market Size
- The global private nursing services market has demonstrated a consistent growth trajectory from 2022 to 2032 at a CAGR of 7%.
- In 2022, the market revenue was $609.7 billion, which increased to $652.4 billion in 2023.
- The forecast for 2032 predicts the market will achieve $1,179.3 billion, reflecting a significant and steady increase over the decade.
Global Private Nursing Services Market Share – By Gender
- The global private nursing services market exhibits a distinct gender distribution in market share.
- As of the latest data, female nurses dominate the market, holding a 65% share, while male nurses account for the remaining 35%.

Key Nursing Workers’ Issues and Industry Trends
Level of Stress Experienced by Registered Nurses During Their Work
- In 2023, registered nurses in the United States reported high-stress levels during their work.
- A significant 56% of respondents indicated experiencing a great deal of stress.
- Additionally, 25% reported feeling a lot of stress, while 15% experienced a moderate amount.
- Only a small proportion of nurses reported lower stress levels, with 3% indicating little stress and just 1% stating they did not feel stressed at all.

Factors Influencing Work Satisfaction Among Nursing Staff
- To increase overall work satisfaction among nursing staff, 68% of respondents indicated that increasing salary, wages, or bonuses would be most effective.
- Additionally, 59% highlighted the need for more nurses or support staff. Addressing nurses’ needs and genuinely listening to their voices was important for 31% of respondents.
- Both increasing nurse recognition and allowing adequate time for meals and breaks were cited by 19% of respondents.
- Offering flexible scheduling was preferred by 16%, while 15% emphasized the importance of being able to take a day off when necessary.
- Implementing a no-tolerance workplace policy was important for 10%, and increasing shared governance was mentioned by 9%.
- Providing more mental health and well-being services was also important for 9%, and 8% of respondents wanted the implementation of innovative technology.
- Creating an anti-bullying policy or program was suggested by 7%, while 6% had other suggestions.
- Providing more housing, transportation, or childcare services was important for 4%, and 3% wanted longer maternity and paternity leave or the opportunity to attend a formal resiliency program.

Regulations for Nursing Workers
- Regulations for nursing workers exhibit significant variation across countries, addressing issues from licensing and practice standards to workplace protections and immigration rules.
- In the United States, state-level legislation often focuses on addressing staffing shortages and improving education funding.
- For example, Alabama’s Preceptor Tax Incentive provides income tax credits to healthcare workers training in rural areas. At the same time, Arizona has allocated $15 million to increase nursing faculty in community colleges and universities.
- In the United Kingdom, new immigration regulations impose stringent conditions on international healthcare workers, including salary thresholds for family visas and increased visa application fees, which could adversely impact recruitment and retention in the healthcare sector.
- Additionally, the Pregnant Workers Fairness Act (PWFA) in the U.S. mandates reasonable accommodations for pregnant, postpartum, and lactating workers. At the same time, the Providing Urgent Maternal Protection (PUMP) for Nursing Mothers Act expands protections for nursing mothers at work.
Discuss your needs with our analyst
Please share your requirements with more details so our analyst can check if they can solve your problem(s)



