Table of Contents
Introduction
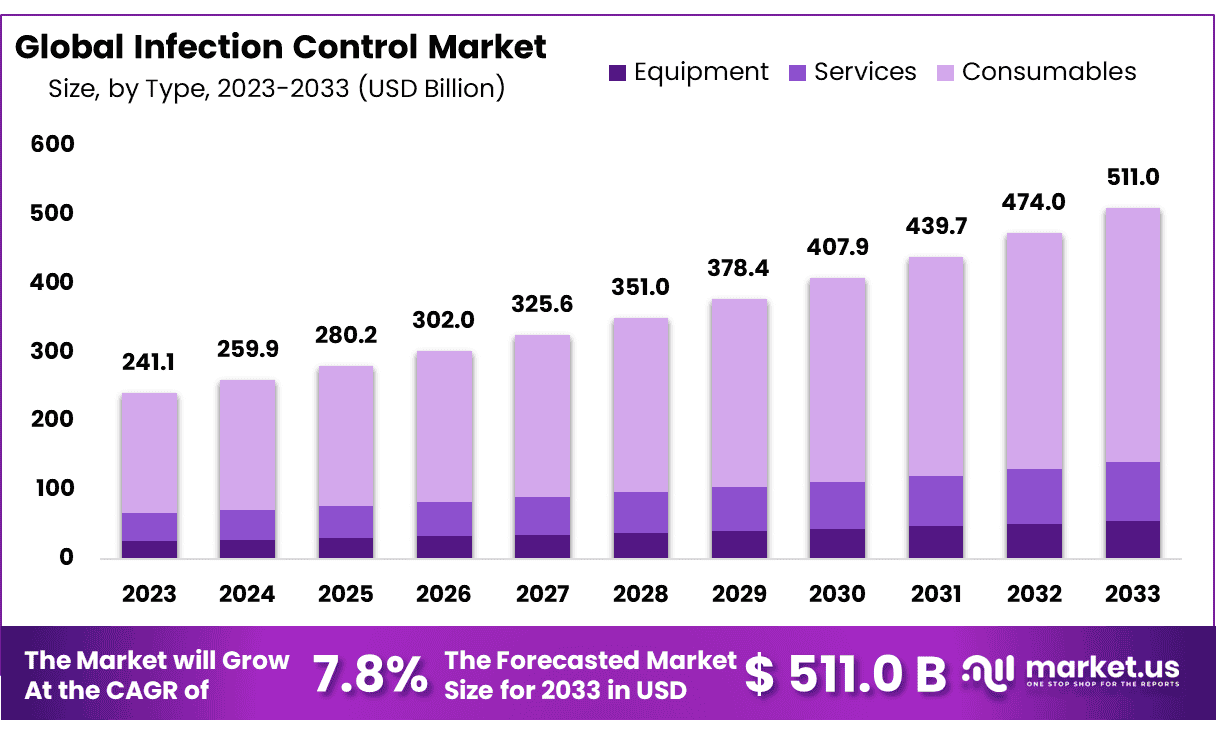
Global Infection Control Market size is expected to be worth around USD 511 Billion by 2033 from USD 241.41 Billion in 2023, growing at a CAGR of 7.8% during the forecast period from 2024 to 2033.
Infection Prevention and Control (IPC) is a crucial discipline that enhances patient safety and healthcare quality by mitigating the risks and spread of healthcare-associated infections (HAIs). This comprehensive field encompasses the prevention of antimicrobial resistance (AMR), positioning it as a vital element in healthcare settings. This module explores the causes of HAIs and the ways in which IPC strategies can effectively reduce their occurrence.
The World Health Organization (WHO) has established core components for IPC based on scientific evidence, expert consensus, and real-world experiences at both national and acute healthcare facility levels. These guidelines are instrumental in strengthening the capacity of Member States to develop and execute technical and behavior-modifying interventions. They are integral to WHO strategies aimed at countering infectious threats like Ebola, enhancing health service resilience, combating AMR, and elevating the overall quality of healthcare delivery.
In conjunction with World Antibiotic Awareness Week (WAAW) 2019, WHO introduced new minimum requirements for IPC programs based on evidence and expert consensus. These requirements serve as a foundational step for countries to develop robust and effective IPC measures at national and facility levels, aiding in the comprehensive adoption of WHO’s IPC recommendations.
Historically, infection control emerged as a formal discipline in the United States during the early 1950s. By the late 1950s and 1960s, an increasing number of hospitals began to acknowledge HAIs and adopted foundational infection control measures. This segment emphasizes the significance of interprofessional teams adhering to infection control principles to enhance healthcare outcomes.Key Takeaways
Infection Control Statistics
- Globally, effective IPC programs can prevent 70% of healthcare-associated infections (HAIs).
- In acute-care hospitals, 7% of patients in high-income countries and 15% in low- and middle-income countries acquire at least one HAI during their stay.
- Approximately 1 in every 10 affected patients will die from their HAI.
- One in four hospital-treated sepsis cases and nearly half of all cases of sepsis with organ dysfunction in adult intensive-care units are healthcare-associated.
- Hand hygiene compliance in healthcare settings remains suboptimal globally, with an average of 59.6%.
- Compliance levels in intensive care units show significant disparity: 64.5% in high-income countries versus 9.1% in low-income countries.
- Hand hygiene improvement programs can prevent up to 50% of avoidable infections acquired during healthcare delivery.
- The economic savings generated by hand hygiene improvement programs average 16 times the cost of implementation.
- Only 3.8% of countries had all minimum requirements for IPC in place at the national level as of 2021–22.
- Only 15.2% of healthcare facilities met all the IPC minimum requirements as per a 2019 WHO survey.
- Antimicrobial resistance increases mortality two to threefold when infections are resistant.
- 24% of patients affected by healthcare-associated sepsis and 52.3% of those in intensive care units die each year.
- Significant progress has been noted in the percentage of countries with a designated IPC focal point, a dedicated budget for IPC, and a curriculum for frontline healthcare worker training.
- The adoption of multimodal strategies for IPC interventions has increased.
- Establishing hand hygiene compliance as a key national indicator is now more common among countries.
Infection Control Type Analysis
Equipment
- Disinfectors: Disinfectors are crucial in maintaining a sterile environment in healthcare settings. These devices range from simple autoclaves to advanced robotic systems that automate the cleaning and disinfection of surgical instruments and other medical devices.
- Endoscope Reprocessors: Endoscope reprocessors are specialized devices designed to ensure the high-level disinfection of endoscopes, which are particularly challenging to clean due to their intricate designs and the need for meticulous handling to prevent healthcare-associated infections.
- Others: Additional critical equipment includes UV-C disinfection robots and air sterilizers that help in reducing airborne and surface pathogens in healthcare environments, thereby minimizing the risk of infection transmission.
Services
- Contract Sterilization: This service provides healthcare facilities with third-party sterilization of equipment, often using technologies such as ethylene oxide or hydrogen peroxide vapor, which are effective in sterilizing a wide range of medical devices without damaging sensitive materials.
- Infectious Waste Disposal: Proper disposal of infectious waste is essential to infection control, involving specialized services that manage the segregation, collection, and disposal of medical waste to prevent contamination and spread of infections.
Consumables
- Infectious Waste Disposal: Items such as biohazard bags and containers are crucial for the safe disposal of infectious waste, helping to contain biohazards right at the source and throughout the disposal process.
- Disinfectants: These are chemical agents used on surfaces and equipment to kill infectious agents. The selection of appropriate disinfectants is based on the specific pathogens present, the area of application, and compatibility with the materials being treated.
- Sterilization Consumables: Consumables like sterilization pouches, indicator strips, and maintenance solutions are vital for ensuring the effectiveness of sterilization processes in healthcare settings.
- Personal Protective Equipment (PPE): PPE includes gloves, gowns, masks, and shields that are essential for protecting healthcare workers from infectious agents during patient care activities. Proper usage and disposal are critical for effective infection control.
- Others: Additional consumables include single-use instruments, custom procedure trays, and cleaning kits that are designed for one-time use to prevent cross-contamination between patients.
Emerging Trends
- Increased Emphasis on Hand Hygiene – Ongoing campaigns like “Clean Hands Count” promote rigorous hand hygiene practices, which are foundational to infection prevention in healthcare settings.
- Use of Personal Protective Equipment (PPE) – Updated guidelines emphasize the proper selection and use of PPE, including respirators and eye protection, especially during aerosol-generating procedures.
- Implementation of Environmental Cleaning Protocols – Enhanced disinfection practices in healthcare facilities aim to prevent the transmission of pathogens on surfaces and medical equipment.
- Antimicrobial Stewardship – Programs to optimize the use of antimicrobial agents continue to expand, aimed at reducing antimicrobial resistance.
- Advancements in Surveillance Technology – The adoption of digital tools and data analytics enhances the monitoring and reporting of hospital-acquired infections.
- Education and Training – Ongoing professional development on infection control practices is crucial, as evidenced by multiple certification and training programs.
- Vaccination Policies – Increasingly, healthcare facilities enforce vaccination policies for staff to prevent outbreaks of vaccine-preventable diseases like influenza and COVID-19.
- Collaboration Across Sectors – Strengthening ties between public health officials, healthcare providers, and policymakers to foster a community-wide approach to infection control.
- Focus on Outpatient Settings – Expanding infection prevention protocols beyond hospitals to include ambulatory and community healthcare settings to reduce widespread transmission.
- Preventive Measures for Specific Settings – Tailored guidelines for unique settings, like long-term care facilities and during specific procedures, to address distinct risks.
Use Cases
- Hand Hygiene Programs: Implementation of hand hygiene programs across healthcare facilities globally has significantly reduced the transmission of pathogens. These programs emphasize the importance of handwashing at critical points during care delivery, drastically lowering the incidence of healthcare-associated infections.
- Surgical Site Infection (SSI) Prevention: Guidelines on managing surgical sites include sterilization and antisepsis protocols which have been effective in reducing SSIs, thereby improving patient recovery times and reducing hospital stays.
- Injection Safety: The implementation of safety protocols for injections and other invasive procedures ensures the minimization of infection risks from contaminated instruments, contributing to safer patient care environments.
- Antimicrobial Stewardship: Programs aimed at optimizing the use of antimicrobial agents improve patient outcomes, reduce microbial resistance, and decrease the spread of infections caused by multidrug-resistant organisms.
- COVID-19 Response: During the COVID-19 pandemic, IPC measures, including the use of personal protective equipment (PPE) and isolation protocols, were crucial in managing and controlling the spread of the virus in healthcare settings.
- Water, Sanitation, and Hygiene (WASH): Implementing WASH programs in healthcare facilities is critical for preventing HAIs, particularly in settings that lack basic sanitation infrastructure.
- Education and Training: Continuous training of healthcare workers on IPC practices helps maintain high standards of infection control, especially in the handling and care of patients in isolation.
- Environmental Cleaning: Regular and thorough cleaning and disinfection of the healthcare environment prevent the spread of infections within facilities, especially in high-risk areas like operating rooms and intensive care units.
- Outbreak Investigations: IPC units are crucial in investigating and managing outbreaks within healthcare facilities, utilizing surveillance data to track infection trends and effectiveness of control measures.
- Policy Development and Implementation: Development of IPC policies based on latest research and tailored to local needs helps in setting up a structured response to infection risks, which is crucial for maintaining overall health security.
Conclusion
Infection Prevention and Control (IPC) is a fundamental aspect of enhancing healthcare quality and safety by preventing the spread of healthcare-associated infections (HAIs) and antimicrobial resistance (AMR). Effective IPC measures, such as rigorous hand hygiene, use of personal protective equipment (PPE), and environmental cleaning protocols, are critical in reducing the incidence of HAIs. These practices not only save lives but also significantly reduce healthcare costs. The World Health Organization’s guidelines and initiatives support global efforts to establish robust IPC strategies, emphasizing the importance of comprehensive training, policy development, and intersectoral collaboration to sustain health security.
Discuss your needs with our analyst
Please share your requirements with more details so our analyst can check if they can solve your problem(s)



