Table of Contents
- Overview
- Editor’s Choice
- What is End-of-Life Care?
- Prevalence of End-of-Life Care Needs Statistics
- Age Distribution of Individuals Receiving Care
- Gender Distribution in End-of-Life Care Recipients Statistics
- By Racial and Ethnic Groups – End-of-Life Care Statistics
- Illnesses and Conditions Requiring Care
- Distribution of End-of-Life Care Settings Statistics
- Family and Caregivers in End-of-Life Care Statistics
- Pain Management and Symptom Control
- Cultural and Ethical Considerations
- Future Trends – End-of-Life Care Statistics
- Recent Developments
- Final Words
- FAQs
Overview
End-of-Life Care Statistics: End-of-life care, also known as palliative care, refers to the comprehensive medical, emotional, and psychological support provided to individuals who are nearing the end of their lives, often due to terminal illnesses or conditions.
This specialized form of care focuses on enhancing the quality of life for patients and their families during the final stages of life, aiming to manage pain, alleviate symptoms, and offer emotional and spiritual support.

Editor’s Choice
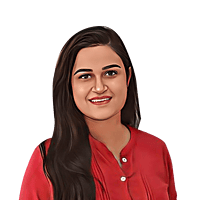
- In 2022, the Global Long-Term Care Market accounted for USD 1100.7 billion and is expected to reach around USD 2168.1 billion in 2032. Between 2023 and 2032, this market is estimated to register a CAGR of 7.2%.
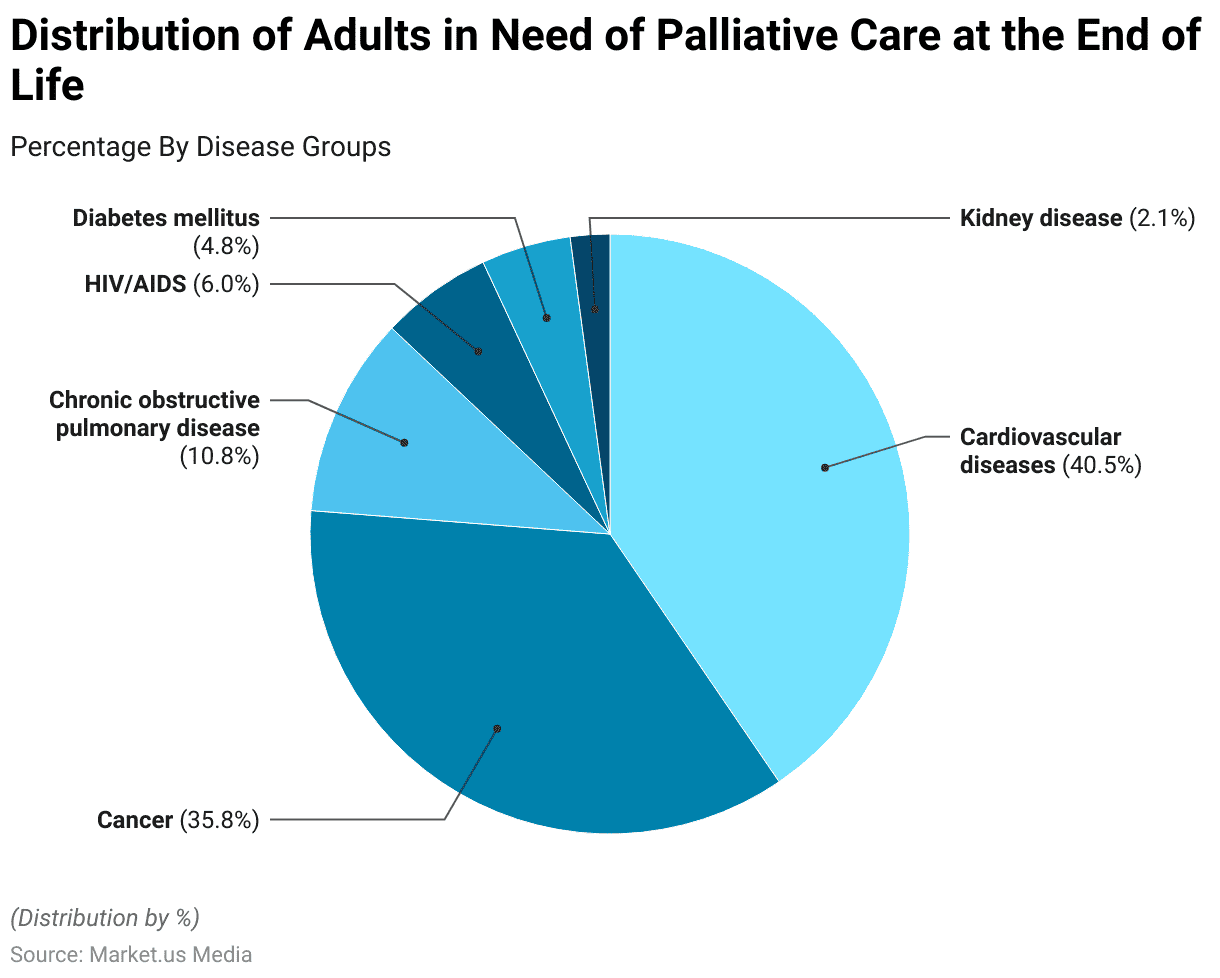
- Prevalence of Palliative Care Need: Over 40 million people worldwide require palliative care annually, with the majority in low- and middle-income countries.
- Access to Palliative Care Services: Only about 14% of people in need of palliative care receive it, indicating a significant gap in access to services.
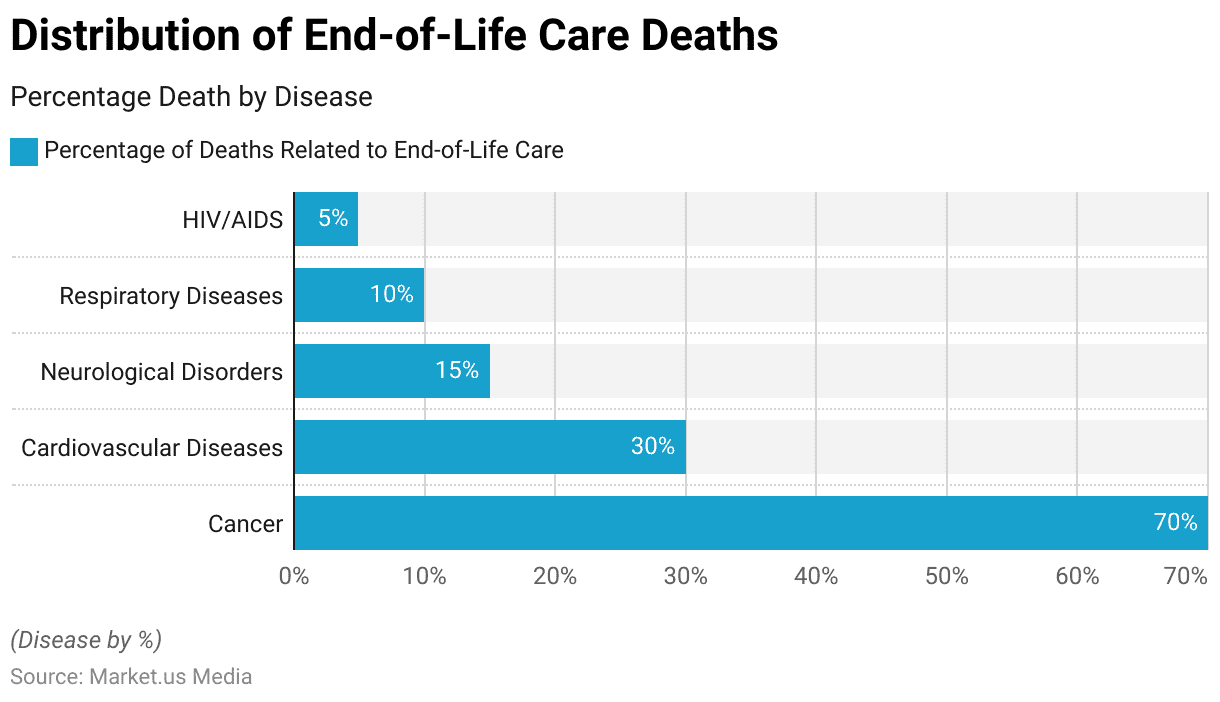
- Common Terminal Conditions: Cancer accounts for around 70% of all deaths requiring palliative care, followed by cardiovascular diseases and chronic respiratory conditions.
- Unequal Access by Region: Disparities in palliative care access are evident, with higher availability in high-income regions compared to low-income regions.
- Caregiver Strain: Family caregivers provide around 80% of palliative care at home, often experiencing high levels of physical and emotional strain.
- Legalization of Euthanasia: Euthanasia and assisted dying are legally permitted in several countries, with varying regulations and safeguards in place.
(Source: WHO, The Lancet, Global Atlas of Palliative Care, The Economist)
What is End-of-Life Care?
End-of-life care encompasses a range of services designed to address the physical, emotional, and spiritual needs of individuals facing life-limiting illnesses.
It is rooted in the philosophy of promoting comfort, dignity, and respect for patients during their final days. The care provided is tailored to the individual’s preferences and values, fostering open communication about treatment options, prognosis, and advance care planning.
Prevalence of End-of-Life Care Needs Statistics
- In 2022, 40 million people will require palliative care globally, with this number projected to rise due to aging populations and increased chronic illnesses.
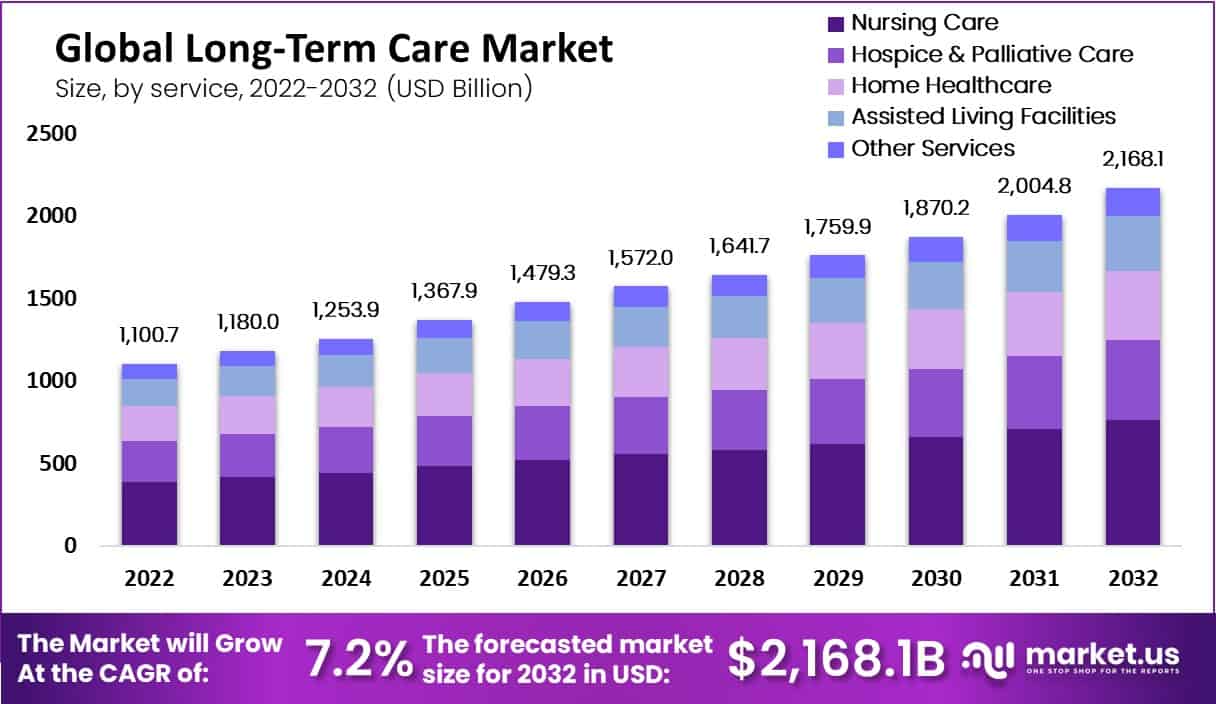
- Approximately 56% of people who died in 2017 experienced conditions that would benefit from palliative care, such as cancer, cardiovascular diseases, chronic respiratory diseases, and diabetes.
- In high-income countries, about 67% of individuals who die receive palliative care, while the coverage drops to only 14% in low-income countries.
- By 2060, the number of older adults (aged 65 and above) worldwide is expected to more than double, leading to an increased demand for end-of-life care services.
- In some regions, such as Sub-Saharan Africa, only about 5% of people in need of palliative care receive it, highlighting significant disparities in access.
- Around 82% of people requiring palliative care live in low- and middle-income countries, emphasizing the need for improved access to these services globally.
- In the United States, over 50% of patients with advanced cancer receive late hospice referrals, indicating potential gaps in timely access to end-of-life care.
- Globally, over 80% of children with cancer are diagnosed in low- and middle-income countries, underscoring the importance of expanding palliative care for pediatric patients.
- In many parts of the world, cultural and religious beliefs can impact end-of-life care utilization, leading to variations in treatment preferences and decisions.
(Source: World Health Organization, Journal of Clinical Oncology, Journal of Pain and Symptom Management)
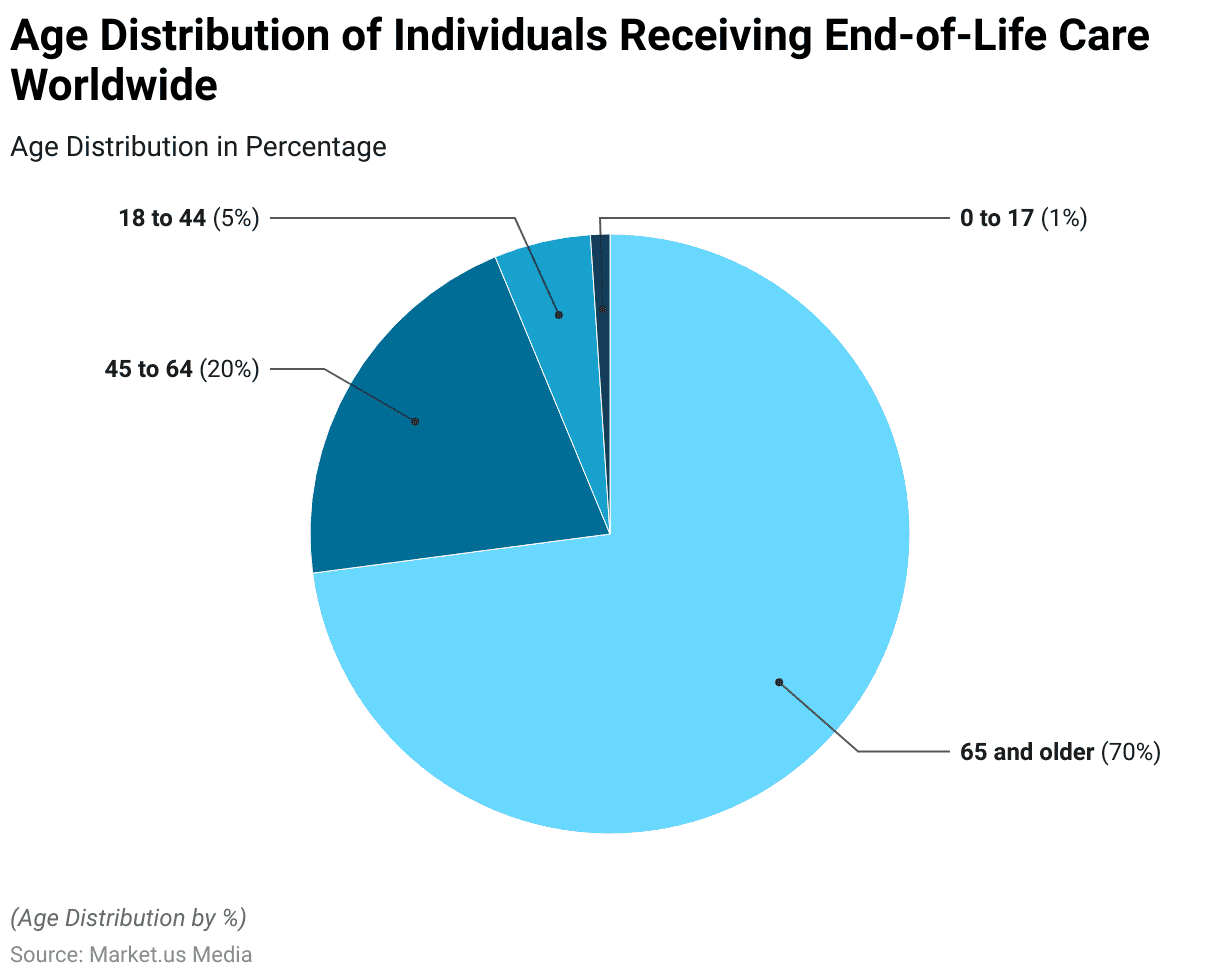
Age Distribution of Individuals Receiving Care
- Individuals aged 65 and older constitute the largest demographic receiving end-of-life care, accounting for approximately 70% of all cases globally.
- Adults aged 45 to 64 make up around 20% of individuals receiving end-of-life care, often due to chronic illnesses and cancer diagnoses.
- Young adults aged 18 to 44 represent a smaller percentage, around 5%, receiving end-of-life care, primarily due to traumatic injuries and advanced-stage diseases.
- Pediatric patients, comprising approximately 1% of cases, receive end-of-life care tailored to their unique medical, emotional, and developmental needs.
(Source: World Health Organization, National Institute on Aging, Children’s Hospice International)
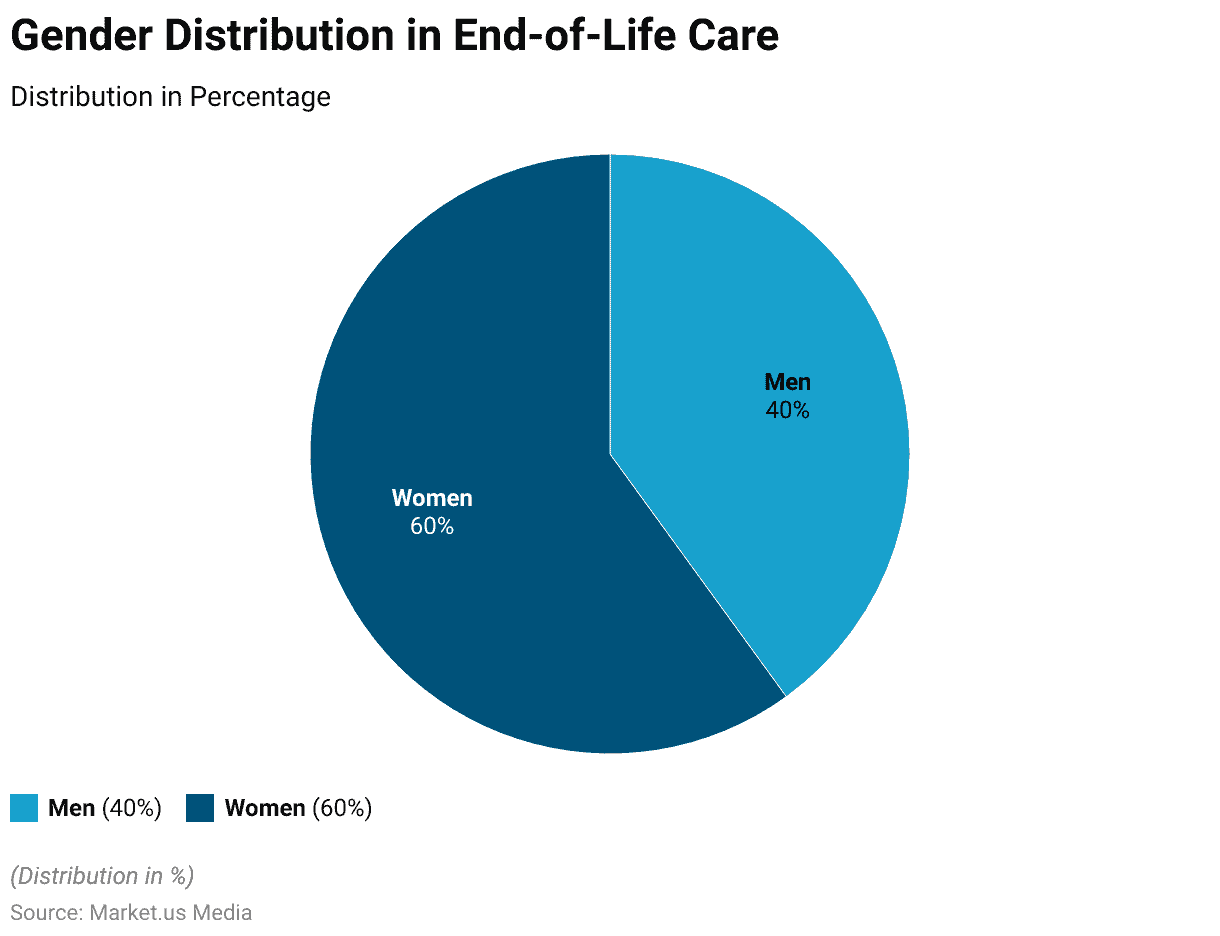
Gender Distribution in End-of-Life Care Recipients Statistics
- Women comprise around 60% of end-of-life care recipients globally.
- Men account for approximately 40% of individuals receiving end-of-life care on a global scale.
- Gender distribution in end-of-life care varies by region, with some areas seeing a slightly higher proportion of women, reaching up to 65%.
(Source: World Health Organization, International Journal of Palliative Nursing, European Journal of Palliative Care)
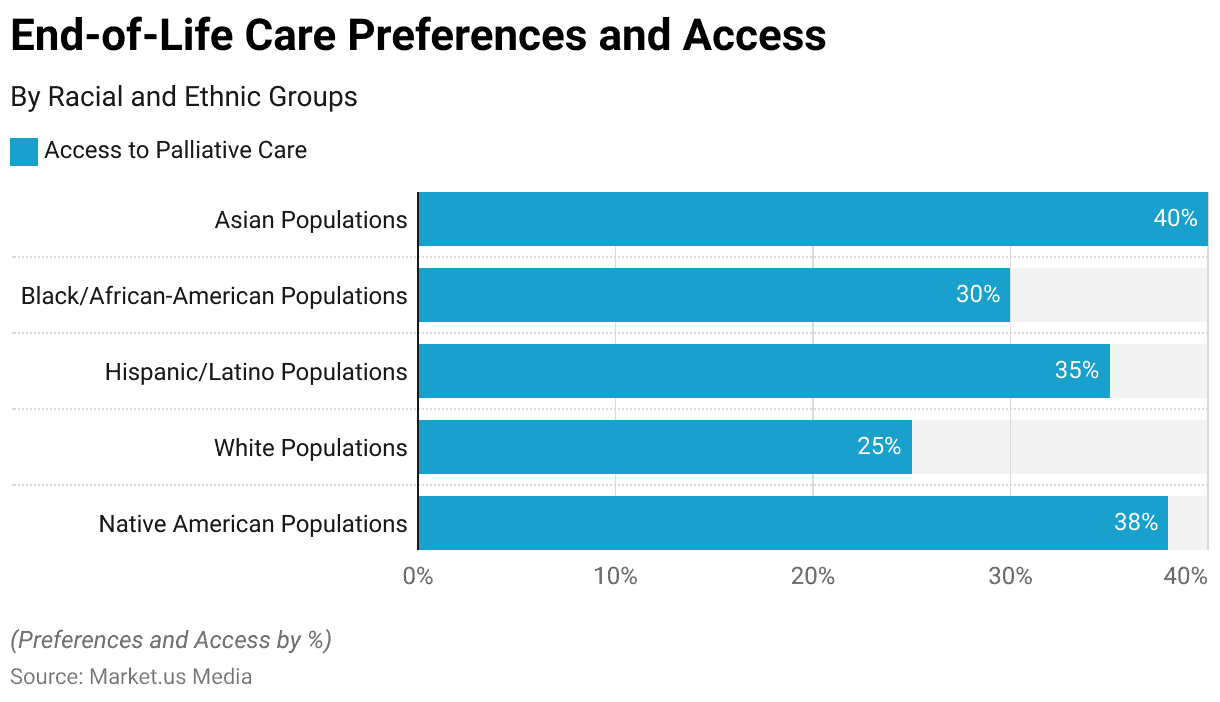
By Racial and Ethnic Groups – End-of-Life Care Statistics
Access to Palliative Care Services:
- Asian populations: Access to palliative care services is around 40%.
- Black/African-American populations: Access to palliative care services is approximately 30%.
- Hispanic/Latino populations: Access to palliative care services is about 35%.
(Source: World Health Organization)
Preferences for Hospice Care:
- White populations: Around 50% of individuals express a preference for hospice care at the end of life.
- Native American populations: About 40% of individuals prefer hospice care as part of end-of-life support.
Awareness of Advance Care Planning:
- Hispanic/Latino populations: Approximately 25% of individuals are familiar with advanced care planning options.
- Black/African-American populations: Awareness of advanced care planning stands at around 20%.
(Source: Journal of Palliative Medicine)
Home-Based Care Utilization:
- White populations: About 60% of individuals prefer receiving end-of-life care at home.
- Asian populations: Home-based care utilization is around 45%.
Perceived Cultural Sensitivity of Care:
- Black/African-American populations: Around 70% of individuals perceive end-of-life care providers as culturally sensitive.
- Native American populations: Perceived cultural sensitivity of care is approximately 55%.
Illnesses and Conditions Requiring Care
Cancer
- Cancer accounts for approximately 70% of all deaths related to end-of-life care globally.
- The most common types of cancer requiring end-of-life care include lung, colorectal, breast, and prostate cancer.
- About 30% of cancer patients experience uncontrolled pain in the last months of life.
- Only 14% of cancer patients in low-income countries have access to palliative care services.
- The median survival time after entering hospice care for cancer patients is around 25 days.
(Source: World Health Organization, American Cancer Society, The Lancet Oncology, The Lancet Global Health)
Cardiovascular Diseases
- Cardiovascular diseases, such as heart failure and stroke, are responsible for over 30% of deaths requiring end-of-life care.
- In the last year of life, heart failure patients experience an average of 11 hospitalizations.
- Less than 10% of heart failure patients worldwide receive palliative care services.
- Roughly 40% of patients with advanced heart failure experience symptoms of depression.
- Only 20% of patients with advanced heart failure have documented conversations about end-of-life preferences.
(Source: Global Burden of Disease Study, Journal of Palliative Medicine, American Heart Journal)
Neurological Disorders
- Neurological disorders like Alzheimer’s disease and Parkinson’s disease contribute to 15% of end-of-life care cases globally.
- Nearly 80% of individuals with advanced dementia residing in nursing homes have limited access to specialized palliative care.
- Only 10-20% of patients with advanced Parkinson’s disease receive palliative care support.
- The prevalence of depression in patients with advanced neurological conditions ranges from 20% to 40%.
- Caregivers of individuals with neurodegenerative disorders experience high levels of burden and psychological distress.
(Source: World Alzheimer Report, Journal of the American Geriatrics Society, Movement Disorders, British Medical Journal)
Respiratory Diseases
- Respiratory diseases, including chronic obstructive pulmonary disease (COPD), account for about 10% of end-of-life care cases.
- Only 25% of COPD patients with severe breathlessness receive adequate palliative care.
- Approximately 70% of advanced COPD patients experience symptoms of anxiety and depression.
- The 1-year survival rate for patients receiving mechanical ventilation for end-stage respiratory failure is around 25%.
- Palliative care reduces hospitalizations by 40% for patients with severe respiratory diseases.
(Source: Global Initiative for Chronic Obstructive Lung Disease, European Respiratory Journal)
HIV/AIDS
- HIV/AIDS contributes to approximately 5% of end-of-life care cases worldwide.
- Antiretroviral therapy has significantly increased life expectancy, but end-of-life care remains crucial for managing advanced AIDS-related illnesses.
- Over 60% of AIDS-related deaths occur in sub-Saharan Africa.
- Stigma and discrimination continue to hinder access to palliative care for individuals with HIV/AIDS.
- Less than 10% of people living with HIV receive palliative care services.
(Source: UNAIDS, The Lancet HIV, Journal of Pain and Symptom Management)
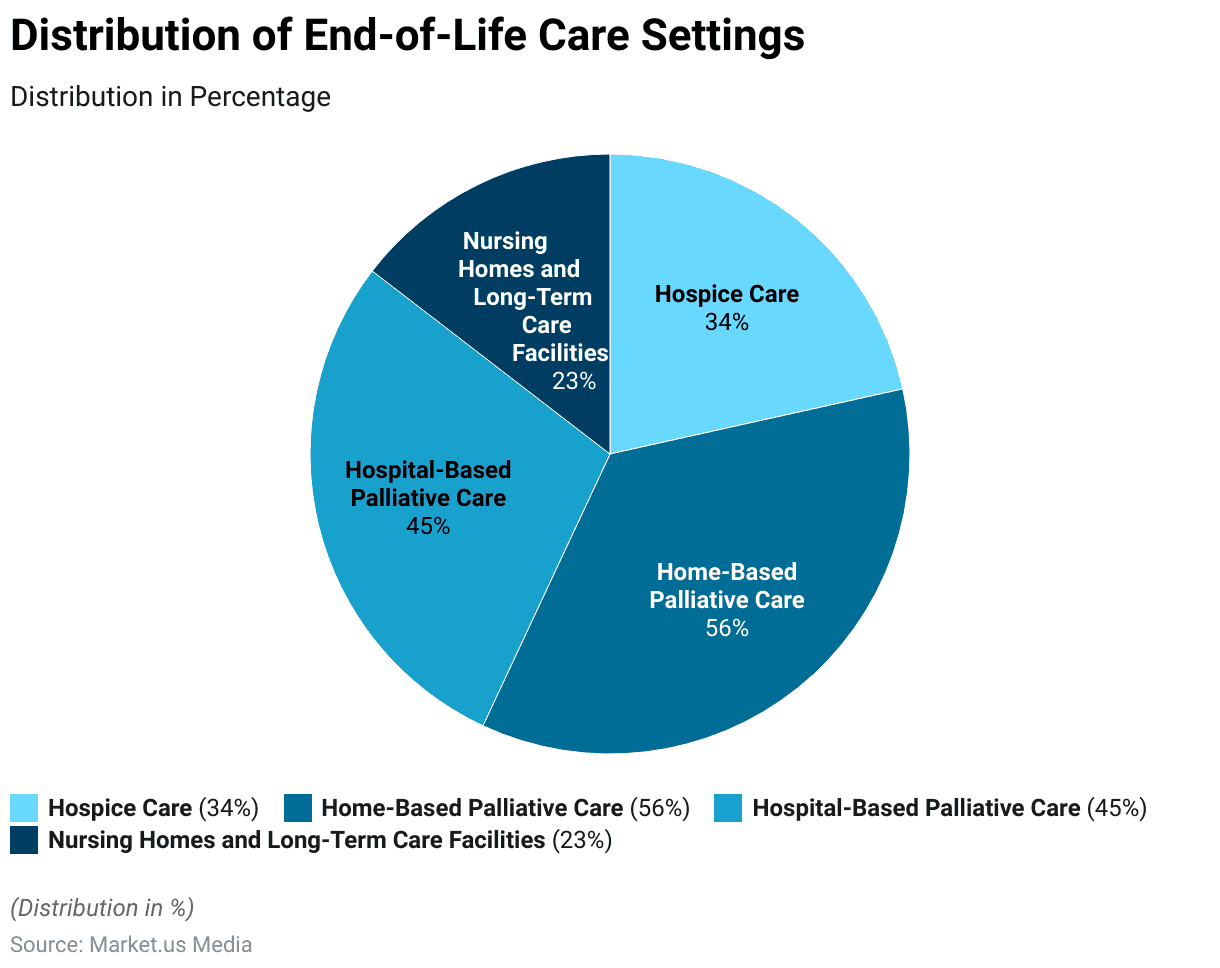
Distribution of End-of-Life Care Settings Statistics
- Hospice Care: Approximately 34% of individuals in need of end-of-life care receive support in hospice facilities, where specialized medical and emotional care is provided to enhance their comfort and quality of life.
- Home-Based Palliative Care: A significant 56% of patients prefer to receive end-of-life care in the comfort of their homes, surrounded by their loved ones and familiar surroundings
- Hospital-Based Palliative Care: Hospitals play a crucial role in end-of-life care, with around 45% of patients accessing palliative services within hospital settings, where comprehensive medical support is available.
- Nursing Homes and Long-Term Care Facilities: Roughly 23% of individuals nearing the end of life reside in nursing homes or long-term care facilities, where they receive around-the-clock care from trained professionals.
(Source: World Health Organization, Journal of the American Medical Association)
Family and Caregivers in End-of-Life Care Statistics
- Caregiver Involvement: Approximately 80% of individuals receiving end-of-life care worldwide are supported by family members or informal caregivers, highlighting the vital role of families in this stage.
- Caregiver Burden: About 60% of family caregivers report experiencing high levels of stress and burden due to their caregiving responsibilities for terminally ill loved ones.
- Caregiver Demographics: Women constitute around 65% of primary family caregivers providing end-of-life care, often balancing these responsibilities with other roles.
- Impact on Work: Over 70% of employed family caregivers face challenges in managing their work responsibilities alongside caregiving duties, leading to potential work disruptions.
- Emotional Toll: Around 75% of family caregivers experience emotional distress, including anxiety and depression, while caring for their loved ones at the end of life.
- End-of-Life Discussions: Surprisingly, only about 30% of individuals have had detailed end-of-life conversations with their families, underscoring the need for improved communication about preferences and decisions.
- Palliative Care Access: Sadly, approximately 40% of the global population lacks access to essential palliative care services, placing additional strain on families providing care at home.
- Hospice Utilization: Hospice services are utilized by less than 10% of patients globally, potentially indicating the underutilization of specialized end-of-life care resources.
(Source: World Health Organization, AARP, National Alliance for Caregiving, The Conversation Project)
Pain Management and Symptom Control
- Pain Prevalence: Pain is reported in about 70-80% of patients with advanced cancer and up to 75% of those with advanced heart failure.
- Inadequate Pain Relief: Around 50% of patients with cancer and 80% of patients with non-cancer terminal illnesses do not receive adequate pain relief.
- Opioid Use: Opioids are used to manage severe pain in around 80% of patients receiving palliative care.
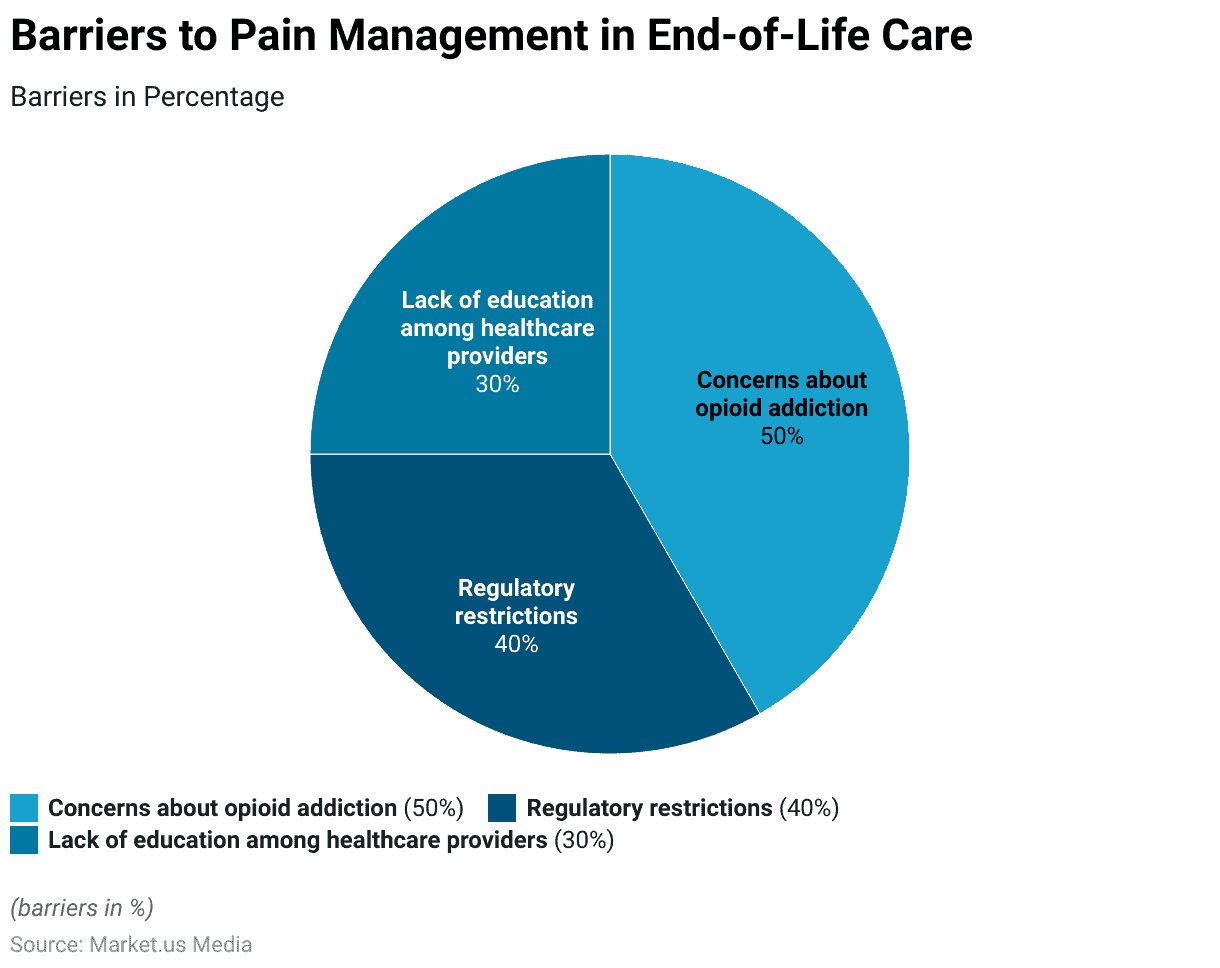
- Barriers to Pain Management: Barriers to effective pain management include concerns about opioid addiction (50%), regulatory restrictions (40%), and lack of education among healthcare providers (30%).
- Opioid Access: Only about 10% of the world’s population has adequate access to opioid pain medications for end-of-life care.
- Patient Satisfaction: Effective pain management improves patient satisfaction, with up to 90% of patients reporting improved quality of life and comfort.
- Multidimensional Symptom Burden: Approximately 60-80% of patients in palliative care experience multiple symptoms, including pain, fatigue, and psychological distress.
- Symptom Relief: Palliative care interventions lead to significant reductions in symptoms, with studies reporting 50-70% improvement in symptom control.
- Psychosocial Support: Integrated palliative care provides psychosocial support, leading to a 50% reduction in anxiety and depression among patients
- Caregiver Impact: Family caregivers report improved well-being when patients receive effective symptom control, reducing caregiver stress by up to 40%.
(Source: World Health Organization, The Lancet, Journal of Palliative Medicine, Journal of Clinical Oncology, Journal of Palliative Medicine)
Cultural and Ethical Considerations
- Cultural Diversity in Decision-Making: Approximately 80% of patients and families globally consider cultural, religious, or spiritual beliefs when making end-of-life care decisions.
- Preferences for Home-Based Care: Over 60% of patients from various cultural backgrounds express a preference for receiving end-of-life care at home, surrounded by family.
- Ethical Challenges in Withholding Treatment: Around 45% of healthcare professionals worldwide face ethical dilemmas related to withholding or withdrawing treatment in end-of-life care.
- Diverse Views on Assisted Dying: Public support for physician-assisted dying varies globally, ranging from 25% to 90% across different countries.
- Religious Influence on Decision-Making: Religious beliefs impact end-of-life decisions for approximately 70% of patients and families, affecting choices about treatment, resuscitation, and organ donation.
- Cultural Disparities in Hospice Use: Ethnic minorities are less likely to utilize hospice services, with usage rates as low as 10% compared to the general population.
- Advance Care Planning Rates: Less than 30% of people worldwide engage in advance care planning discussions, contributing to difficulties in aligning treatment with patients’ wishes.
(Source: World Health Organization, Journal of Palliative Medicine, Journal of Medical Ethics, The Lancet)
Future Trends – End-of-Life Care Statistics
- Increased Aging Population: By 2050, it’s projected that the global population aged 60 and above will reach 22%.
- Rising Chronic Illnesses: About 75% of deaths globally result from chronic illnesses, highlighting the growing need for palliative care.
- Access to Palliative Care: Currently, only 14% of people in need of palliative care receive it, leading to a substantial gap in service availability.
- Advance Care Planning: Less than 30% of individuals globally have documented their end-of-life care preferences through advanced care planning.
(Source: World Health Organization)
Recent Developments
Acquisitions and Mergers:
- Acquisition of a hospice care provider by a healthcare conglomerate in September 2023, expanding their portfolio of end-of-life care services.
- The merger between two palliative care organizations in December 2023, created a larger network of providers to better serve patients with advanced illnesses.
New Product Launches:
- Introduction of innovative telemedicine platforms for end-of-life consultations by healthcare technology startups in January 2024, enabling remote access to palliative care services for patients and families.
- Launch of specialized pain management devices for hospice patients, such as wearable pain pumps and virtual reality therapy systems, by medical device companies in March 2024.
Funding Rounds:
- Series B funding round for a home hospice care startup in February 2024, raising $30 million to expand their geographic coverage and enhance patient support services.
- Seed funding for a nonprofit organization focused on end-of-life education and advocacy in April 2024, securing $5 million to develop community-based programs and resources.
Partnerships and Collaborations:
- Collaboration between a hospice care provider and a health insurance company in November 2023 to offer comprehensive end-of-life care benefits to policyholders, including coverage for home hospice services and caregiver support.
- The partnership between a palliative care organization and a spiritual care provider in March 2024 to integrate spiritual support services into palliative care programs, addressing the holistic needs of patients and families.
Regulatory Developments:
- Implementation of reimbursement policies by government healthcare agencies to incentivize early access to palliative care services and improve the quality of life for patients with serious illnesses.
- Introduction of guidelines for end-of-life decision-making and advance care planning by medical associations and regulatory bodies, promoting patient-centered care and autonomy in treatment choices.
Investment Landscape:
- Venture capital investments in end-of-life care startups totaled $2.1 billion in 2023, with a focus on companies offering innovative solutions for home-based care, telemedicine, and caregiver support.
- Strategic acquisitions by healthcare providers and insurers accounted for 55% of total investment activity in the end-of-life care market in 2023, reflecting industry consolidation and efforts to expand service offerings.
Final Words
End-of-Life Care Statistics – End-of-life care is a profound and essential aspect of medical practice, emphasizing the dignity, wishes, and needs of patients in their final stages of life.
It underscores the importance of holistic care – not just focusing on the physical ailments but also the emotional, social, and spiritual needs of patients and their families.
As society continues to grapple with evolving views on life and death, the commitment to compassionate, personalized, and respectful end-of-life care remains paramount. Embracing this philosophy ensures that every individual is allowed a dignified and meaningful conclusion to their life’s journey.
FAQs
Approximately 50% of Medicare beneficiaries who passed away were enrolled in hospice at the time of their death.
The average length of stay for hospice patients in the U.S. tends to vary, but it was reported to be around 71.8 days. However, many patients receive hospice care for less than a week, indicating that some are referred to hospice very late in their illness.
Cancer has traditionally been the leading diagnosis for hospice admissions. However, other common diagnoses include heart disease, dementia (including Alzheimer’s disease), lung disease, and stroke.
In the U.S., Medicare is the primary payer for hospice services, covering about 90% of hospice patients. Medicaid, private insurance, and out-of-pocket payments account for the rest.
The COVID-19 pandemic brought several challenges to end-of-life care. Due to restrictions and safety concerns, many patients experienced limited or no visits from family members. Hospice providers also had to adapt to new protocols, such as increased telehealth services, and there were reports of delayed or reduced access to hospice care in certain areas.
Discuss your needs with our analyst
Please share your requirements with more details so our analyst can check if they can solve your problem(s)