Table of Contents
Introduction
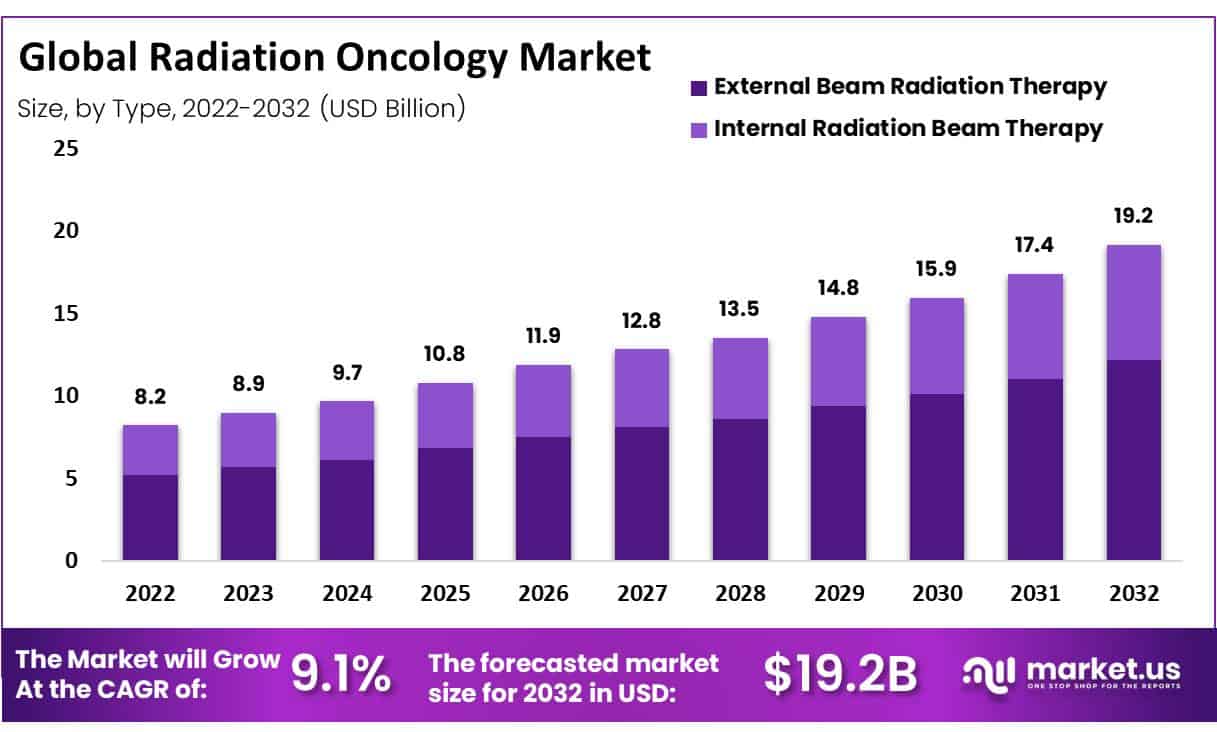
Global Radiation Oncology Market size is expected to be worth around USD 19.2 Billion by 2032 from USD 8.9 Billion in 2023, growing at a CAGR of 9.1% during the forecast period from 2024 to 2032.
The global radiation oncology market is experiencing significant growth driven by the increasing prevalence of cancer worldwide, influenced by aging populations, lifestyle changes, and environmental factors. Radiotherapy plays a crucial role in cancer treatment, with nearly 50% of patients undergoing it as part of their treatment regimen, and it contributes to 40% of curative treatments. The therapeutic benefits of radiotherapy, coupled with technological advancements such as intensity-modulated radiation therapy (IMRT), stereotactic radiosurgery (SRS), and proton therapy, have greatly improved treatment precision and patient outcomes.
Additionally, the integration of radiation therapy with chemotherapy and surgery in combination therapies has broadened treatment options, enhancing the efficacy of cancer care. The demand for radiation therapy products is further fueled by rising government spending on healthcare and the opportunities emerging from developing economies.
According to the World Health Organization, the most prevalent cancers in 2020 included breast, lung, and colorectal, with respective case counts of 2.26 million, 2.21 million, and 1.93 million. The American Cancer Society estimates around 1.9 million new cancer diagnoses in the U.S. for 2022. Furthermore, the Global Cancer Observatory reported significant regional disparities in cancer incidence for 2022, with Asia accounting for 49.2% of cases, followed by Europe at 22.4%, Latin America at 13.4%, the Caribbean at 7.8%, and other regions comprising 7.2%.
Key Takeaways
- Market Size: Radiation Oncology Market size is expected to be worth around USD 19.2 Billion by 2032 from USD 8.9 Billion in 2023.
- Market Growth: The market growing at a CAGR of 9.1% during the forecast period from 2023 to 2032.
- Type Analysis: The external beam therapy segment accounted for the highest market revenue share of 63.4% in 2022.
- Indication Analysis: The breast cancer segment dominated the maximum market revenue share of 34% in 2022.
- End-Use Analysis: The the hospital’s segment dominated the highest market revenue share in 2022.
- Regional Analysis: North America accounted for a significant radiation oncology market revenue share of 43.5% in 2022.
- Market Expansion: The market is expanding due to increasing healthcare expenditures, government funding, and investments in healthcare infrastructure, particularly in developing countries.
- Collaborative Approaches: There’s a trend towards combination therapies, integrating radiation oncology with surgery and chemotherapy to optimize cancer care.
Radiation Oncology Statistics
- Global Research Output: Asia accounts for 59.5% of the global population but contributes only 21% of the global research output in radiation oncology.
- Cancer Cases by Region: Asia bears nearly 50% of global cancer cases, with cancer incidence at 49.3% in Asia, 22.8% in Europe, and 20.9% in the Americas.
- Radiation Oncology Clinical Trials: Radiation oncology clinical trials make up only 9% of all global oncology randomized controlled trials. Low- and middle-income countries (LMICs) in Asia lead just 13% of these trials globally.
- Common Research Types: Retrospective audits (80%) and observational studies (75%) are the most common research methods conducted in radiation oncology centers.
- Hindrances to Research: The most common barriers to conducting research include lack of time (80%), lack of funding (75%), and limited training in research methodology (40%).
- Preferred Research Areas: Head and neck cancers (45%) and gynecological cancers (25%) are the most preferred disease sites for research among radiation oncology institutions.
- Potential Research Collaboration Areas: Advanced external beam radiotherapy implementation (40%) and cost-effectiveness studies (35%) were identified as promising areas for collaboration.
- Research Training: 75% of respondents had formal research training in radiation oncology, indicating a solid foundation in research skills.
- Active Research Environment: Only 50% of radiation oncology members reported the existence of an active research environment in their country, and 45% expressed a desire to further develop it.
- Publication in Radiation Oncology: Only 5%–20% of radiation oncologists are actively publishing independently, highlighting the need for greater publication efforts.
Emerging Trends
- Hypofractionation: This approach involves administering higher doses of radiation over fewer sessions, aiming to reduce overall treatment time while maintaining efficacy. This method is increasingly favored for its efficiency and effectiveness in managing certain types of cancer.
- Integration of Advanced Imaging: Technologies like MRI-guided radiation therapy are improving the precision of radiation delivery, allowing real-time imaging to better target tumors and spare healthy tissue.
- Proton Therapy: This form of therapy is noted for its precision in targeting tumors while minimizing damage to surrounding healthy tissues, making it particularly useful for complex cancer cases.
- Stereotactic Radiosurgery (SRS): SRS is gaining traction for its ability to deliver precise radiation doses in a single or few sessions, which is crucial for treating small or hard-to-reach tumors.
- Artificial Intelligence and Machine Learning: These technologies are being increasingly utilized to optimize treatment plans, predict patient outcomes, and personalize radiation therapy protocols, enhancing both the effectiveness and safety of treatments.
- Increased Use of Combination Therapies: There is a growing trend towards integrating radiation therapy with chemotherapy and surgical interventions to provide a comprehensive treatment approach that addresses various aspects of cancer management.
- Radiation Therapy Accessibility: Efforts are being made to increase the availability of advanced radiation therapy techniques in developing regions, expanding access to high-quality cancer care globally.
- Focus on Minimizing Side Effects: Modern radiation therapy techniques are increasingly aimed at reducing the side effects associated with radiation, thereby improving the quality of life for cancer patients during and after treatment.
- Expanding Training and Education: Educational initiatives are being enhanced to prepare the next generation of oncologists with the skills needed to utilize advanced radiation technologies and approaches effectively.
- Personalized Radiation Therapy: Tailoring radiation doses and techniques to individual patient profiles is becoming more common, allowing for treatments that are specifically designed based on the genetic and molecular characteristics of both the tumor and patient.
Use Cases
- Basal and Squamous Cell Skin Cancers: Radiation therapy is utilized when surgical options are limited due to the size or location of the tumor, or in patients who are not ideal candidates for surgery.
- Glioblastoma: Tailored radiation therapy regimens are critical in treating aggressive brain tumors like glioblastoma, where precision in targeting the cancerous tissue is paramount for patient outcomes.
- Lower Gastrointestinal Cancers: For cancers of the colon, rectum, and anus, radiation therapy is part of the treatment process, aiding in tumor reduction before surgery or as a primary treatment to manage symptoms and control tumor growth.
- Prostate Cancer: Radiation therapy, including external beam and brachytherapy, is a cornerstone of prostate cancer treatment, providing targeted tumor control with options for varying intensities and durations based on tumor characteristics and patient needs.
- Upper Gastrointestinal Cancers: In cancers involving the esophagus, stomach, liver, and pancreas, radiation therapy plays a crucial role in shrinking tumors and enhancing the effectiveness of surgical and chemotherapeutic interventions.
- Palliative Care for Advanced Cancers: Radiation oncology is not just curative but also extensively used for palliative care, helping manage pain and other symptoms in patients with advanced cancer, thereby improving quality of life.
- Breast Cancer: Radiation therapy post-mastectomy or lumpectomy helps destroy any remaining cancer cells, significantly reducing the risk of recurrence and is a standard part of breast-conserving therapy.
- Head and Neck Cancers: In cancers of the oral cavity, throat, and larynx, radiation therapy is effective both as a primary treatment and in conjunction with surgery and chemotherapy, tailored to preserve organ function and reduce cosmetic impact.
- Brain Metastases: Stereotactic radiosurgery, a form of radiation therapy, provides a non-invasive treatment option for patients with metastatic brain tumors, offering precise targeting with minimal impact on surrounding healthy tissue.
- Pediatric Cancers: Radiation therapy is used with caution in pediatric oncology due to the sensitivity of developing tissues but remains integral in cases where tumor reduction can significantly impact survival and quality of life outcomes.
Conclusion
The global radiation oncology market is set to expand significantly, with projections estimating its growth from USD 8.9 billion in 2023 to USD 19.2 billion by 2032, at a CAGR of 9.1%. This growth is fueled by the increasing incidence of cancer globally, advancements in radiation therapy technologies, and the integration of these treatments with other cancer care methods.
Technological innovations like intensity-modulated and stereotactic radiosurgery, along with proton therapy, are enhancing the precision and efficacy of treatments, contributing significantly to curative outcomes. Additionally, the development of combination therapies and increasing healthcare investments in developing regions are pivotal in broadening the scope and accessibility of radiation oncology services. The market’s expansion is also supported by a growing focus on minimizing treatment side effects and improving patient quality of life through advanced therapeutic approaches.
Discuss your needs with our analyst
Please share your requirements with more details so our analyst can check if they can solve your problem(s)



