Table of Contents
Introduction
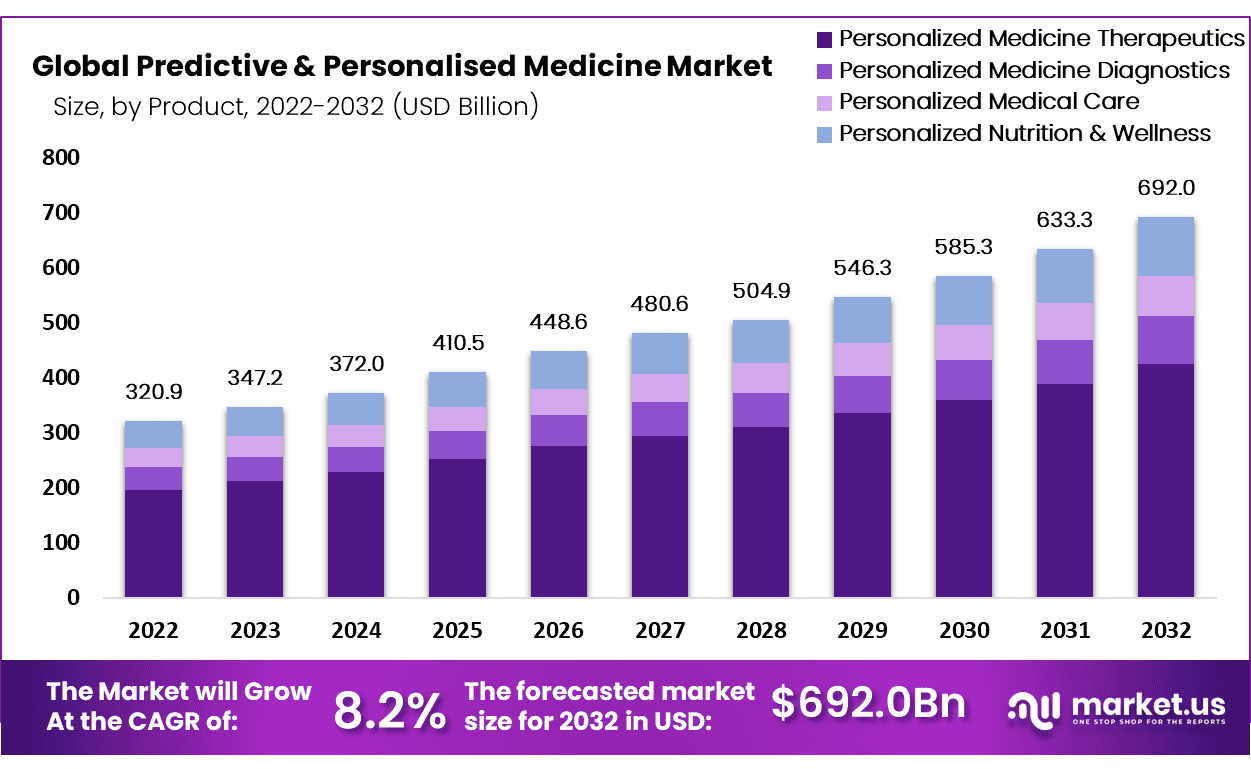
Global Predictive & Personalized Medicine Market size is expected to be worth around USD 692.0 Billion by 2032 from USD 347.2 Billion in 2023, growing at a CAGR of 14.2% during the forecast period from 2024 to 2032.
Predictive and personalized medicine stands at the forefront of a healthcare revolution, offering treatments specifically tailored to individual genetic profiles, environmental factors, and lifestyle choices. This approach utilizes cutting-edge genomics and biotechnology to predict disease risks and enhance the efficacy of treatments, centering on genetic testing to identify unique biomarkers. These biomarkers are crucial for determining how individuals respond to drugs and their susceptibility to certain diseases.
With the aid of big data analytics, predictive and personalized medicine can sift through vast health data sets to deliver more accurate and effective medical interventions. This shift towards customized healthcare is largely driven by the rising prevalence of genetic disorders, an aging global population, and a growing preference for targeted therapeutic approaches.
Despite its promising prospects, the field faces significant challenges, including privacy issues related to genetic information, the high costs associated with genetic testing, and the necessity for robust clinical validation. Nonetheless, the potential to reduce adverse drug reactions and enhance the efficiency of healthcare systems offers substantial incentives for continued investment and development in this area.
Predictive and personalized medicine not only promises a transition from reactive to proactive treatments but also has the potential to significantly improve patient outcomes and the overall effectiveness of healthcare systems worldwide.
Key Takeaways
- Market Size: Global Predictive & Personalized Medicine Market size is expected to be worth around USD 692.0 Billion by 2032 from USD 347.2 Billion in 2023.
- Market Growth: The market growing at a CAGR of 14.2% during the forecast period from 2024 to 2032.
- Product Analysis: The personalized nutrition and wellness segment held the highest share.
- Application Analysis: High prevalence of cancer results in the growth of the oncology segment
- End-Use Analysis: High procedural volume in hospitals & clinics will drive the market’s growth.
- Regional Analysis: North America dominated the market with the largest share of 47.2% in 2022.
- Technological Integration: Integration of technologies such as machine learning, AI, and blockchain is enhancing data analysis capabilities, leading to better patient outcomes and optimized treatment protocols.
- Challenges in Implementation: Despite the advancements, there are challenges related to data privacy, high costs of personalized therapies, and the need for more robust healthcare IT infrastructures to handle complex data.
Predictive & Personalized Medicine Statistics
- Personalized Medicine Approvals by FDA: In the last decade, over 25% of newly approved drugs by the FDA are classified as personalized medicines, illustrating the growing adoption of tailored therapies in healthcare.
- New Drug Approvals in 2023: In 2023, 20 personalized medicines were approved, representing 38% of all new therapeutic molecular entities approved by the FDA.
- Predictive Model Accuracy: A recent study used 2.1 billion measurements from 92 different lab tests to improve disease risk prediction. This data collection increased the predictive accuracy of certain chronic conditions by up to 60%.
- Approval of Gene and Cell Therapies: In 2023, 6 new gene or cell-based therapies were approved for treating conditions such as hemophilia and sickle cell disease.
- Reducing Failure Rates of Standard Treatments: Personalized medicine has been shown to potentially reduce the 40% failure rate of standard treatments by using therapies tailored to an individual’s genetic makeup.
- Clinical Trial Integration: It is predicted that by 2030, 90% of clinical trials will incorporate some form of personalized medicine.
- Cost Reduction Potential: Predictive models using personalized data are expected to lead to a 20% decrease in overall healthcare costs by optimizing treatments and minimizing ineffective interventions.
- Genetic Testing for Early Detection: For genetic conditions such as Lynch syndrome, genetic testing improves early detection and prevention in 85% of cases, allowing for timely medical intervention.
- Electronic Medical Records (EMR) in Predictive Models: The use of electronic medical records (EMR) supports over 70% of predictive models, playing a crucial role in personalized medical approaches.
- Predictive Capabilities of Machine Learning: Machine learning algorithms can now explain more than 50% of test variances for chronic conditions, contributing significantly to personalized treatment plans.
- Faster Drug Efficacy Determination: Precision medicine trials can determine drug efficacy 50% faster than traditional methods, helping to expedite the delivery of effective treatments.
- Reduced Diagnostic Errors: Personalized medicine’s integration into clinical decision-support systems has resulted in a 30% reduction in diagnostic errors.
- Genome-Wide Association Studies (GWAS): Genome-wide association studies have a 60% success rate in identifying specific disease risk factors, aiding in more precise medical interventions.
- Adoption of Personalized Medicine by Healthcare Providers: In the U.S., 43% of healthcare providers have integrated some form of personalized medicine into routine practice.
- Targeted Cancer Therapies: 60% of cancer patients now benefit from targeted therapies informed by genetic profiling, leading to improved outcomes.
- Investment in Predictive Medicine Research: The U.S. government invested $1.5 billion in predictive medicine research in 2022, emphasizing its importance in modern healthcare.
- Prevention of Healthcare Costs: Predictive tools are expected to mitigate or prevent 70% of disease-related healthcare costs by 2030, highlighting their economic benefits.
- Enhanced Diagnostic Capability: Personalized medicine enhances diagnostic capabilities by utilizing molecular information, wearables, and mobile health apps, contributing to better disease management.
Predictive & Personalized Medicine Product Analysis
- Personalized Medicine Therapeutics: Personalized therapeutics utilize genomic and clinical data to tailor treatments to individual patient profiles, significantly enhancing treatment efficacy and reducing side effects. The integration of pharmacogenomics in healthcare allows for the optimization of drug therapy based on individual genetic makeup, ensuring that patients receive the most effective and safe medications tailored to their genetic profile. This approach not only improves patient outcomes but also reduces healthcare costs by minimizing adverse drug reactions and ineffective treatments.
- Personalized Medicine Diagnostics: Advancements in personalized diagnostics are transforming patient care by enabling the early detection and precise targeting of diseases. Molecular diagnostics and biomarker-driven strategies are particularly pivotal in cancer care, where they guide the selection of targeted therapies based on the genetic mutations of a patient’s tumor. This specificity increases the success rate of treatments and spares patients from the side effects of ineffective therapies. The integration of these diagnostics into routine medical practice continues to grow, driven by their potential to significantly improve clinical outcomes.
- Personalized Medical Care: Personalized medical care integrates predictive analytics with traditional medical practices to provide care that is specifically tailored to individual patient needs. This approach leverages comprehensive data analysis, including genetic, environmental, and lifestyle factors, to predict disease risk and tailor prevention strategies accordingly. Personalized medical care is particularly effective in managing chronic diseases and improving health outcomes by enabling proactive rather than reactive medical interventions.
- Personalized Nutrition and Wellness: Personalized nutrition and wellness programs are designed to optimize individual health outcomes based on genetic, metabolic, and gut microbiome analyses. These programs tailor dietary and lifestyle recommendations to improve personal health metrics and prevent nutrition-related diseases. The growing body of research supporting the efficacy of personalized nutrition is driving its adoption, as it demonstrates significant potential in managing weight, enhancing athletic performance, and preventing lifestyle-related diseases such as diabetes and cardiovascular disorders.
Emerging Trends
- Integration into Healthcare Systems: Personalized medicine is being integrated into healthcare systems through a strategic roadmap developed by the International Consortium for Personalised Medicine (ICPerMed). This roadmap outlines how personalized medicine will center around individual characteristics to enhance health outcomes and optimize healthcare efficiency by 2030.
- Bi-Directional Information Flow: There is a growing emphasis on creating a continuous loop of knowledge that integrates research with clinical practice. This integration allows for personalized medicine to be applied effectively in clinical settings, enhancing decision-making and treatment precision. This approach is seen as essential for personalizing care at every level of health status.
- Gene and Cell-Based Therapies: Advances in gene and cell-based therapies continue to make significant impacts, particularly in treating genetic disorders and specific cancer types. These therapies work by altering the molecular pathways associated with diseases, providing long-term benefits and, in some cases, permanent cures.
- Enhanced Molecular Testing: Molecular testing has evolved to pinpoint more accurate therapeutic targets within personalized medicine. This has led to better patient outcomes, especially in oncology, where knowledge about genetic mutations and biomarkers has expanded the use of targeted therapies.
- Patient Adherence to Treatment: Personalized therapies that are more effective and have fewer side effects are improving patient adherence, particularly in chronic disease management. Knowing one’s genetic predisposition can motivate patients to adhere more strictly to treatment regimens, significantly impacting health outcomes.
- Non-Invasive Molecular Tests: The trend towards non-invasive testing continues to grow, with molecular tests that require only a blood sample becoming more common. These tests are replacing more invasive procedures like tissue biopsies, making it easier and less burdensome for patients to undergo testing and monitoring for various conditions.
Use Cases
- Chronic Disease Management: Advanced AI technologies are leveraged to monitor and manage chronic diseases like diabetes in real-time. By analyzing continuous glucose monitoring data, AI can recommend personalized diet and medication adjustments to better manage blood sugar levels, enhancing patient outcomes and reducing healthcare costs.
- Predicting Drug Side Effects: Machine learning models can predict potential side effects from drug interactions. For example, these models assess how a patient’s unique immune system might react to new medications, helping healthcare providers choose safer, more effective treatment options that minimize adverse effects.
- Accelerating Drug Discovery and Repurposing: AI-driven platforms significantly reduce the time and cost associated with drug discovery by analyzing vast chemical libraries to predict drug interactions and efficacy. This technology was notably beneficial in the rapid development of COVID-19 vaccines.
- Early Disease Detection and Risk Stratification: Predictive analytics are used to identify patients at high risk for diseases like breast cancer through the analysis of diagnostic images like mammograms. Early detection enables timely and targeted interventions, improving patient prognoses and potentially saving lives.
- Personalized Treatment Plans: Utilizing diverse health data from large-scale research initiatives like the NIH’s All of Us Research Program, predictive analytics can develop highly tailored treatment plans. This approach considers a patient’s genetic profile, lifestyle, and existing health conditions to optimize therapy.
- Improving Healthcare Operational Efficiency: Predictive analytics help streamline healthcare operations, such as optimizing surgery schedules and managing hospital staff effectively. For instance, predictive models can forecast surgery durations, improving the utilization of operating rooms and reducing patient wait times.
Conclusion
Predictive and personalized medicine is reshaping the landscape of healthcare by delivering customized treatments that optimize patient outcomes and operational efficiency. With a strong foundation in genomics and big data analytics, this approach promises to enhance the precision of medical interventions. However, challenges such as data privacy, high costs, and the need for robust infrastructure persist. Despite these hurdles, the continued advancement in technologies like AI and molecular testing fosters a transformative shift towards proactive healthcare. By embracing these innovations, the healthcare industry can significantly improve treatment efficacy and reduce healthcare costs, paving the way for a more sustainable and effective healthcare system.
Discuss your needs with our analyst
Please share your requirements with more details so our analyst can check if they can solve your problem(s)



