Table of Contents
Introduction
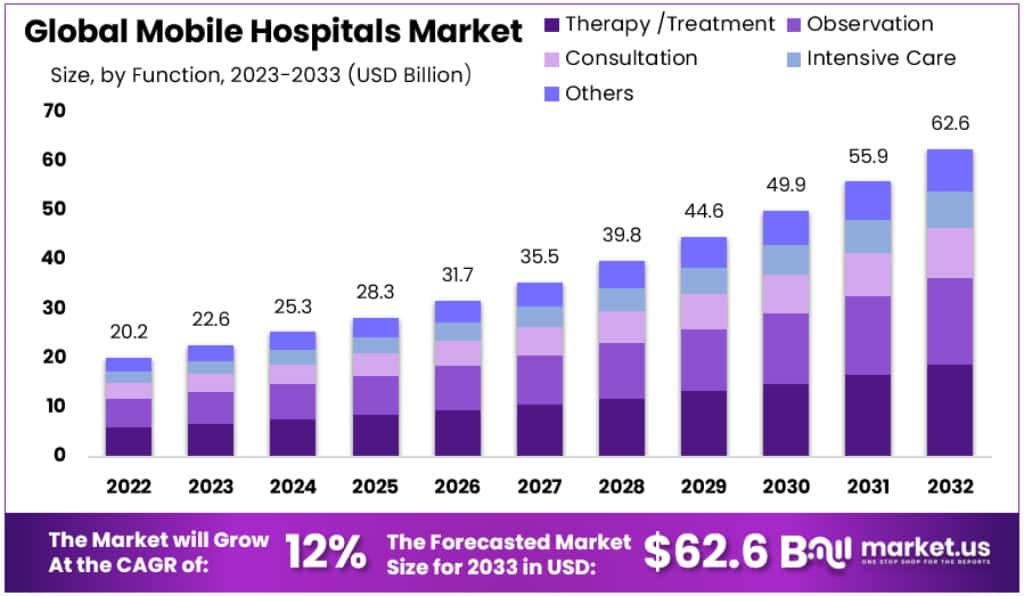
The Global Mobile Hospitals Market is projected to expand significantly, with an estimated value of USD 62.6 billion by 2033, up from USD 22.6 billion in 2023. This growth, expected at a Compound Annual Growth Rate (CAGR) of 12%, is largely driven by technological advancements, government initiatives, and an increasing emphasis on accessible healthcare in remote locations.
Technological enhancements have notably improved mobile hospitals by integrating advanced medical technologies and telemedicine capabilities. This allows for real-time consultations with specialists, particularly crucial in emergency care scenarios. Additionally, cost-effectiveness is a pivotal advantage of mobile hospitals. Compared to traditional facilities, these mobile units require less capital investment and operational costs, making them a preferred choice for extending healthcare services efficiently.
Government support plays a crucial role in the proliferation of mobile hospitals. For example, the Department of Veterans Affairs has developed extensive mobile healthcare services to ensure veterans receive timely care. Such initiatives are bolstered by federal and state funding, highlighting a governmental commitment to healthcare accessibility. Moreover, mobile hospitals are indispensable in disaster response, swiftly providing essential services during emergencies without relying on local infrastructure.
The market’s growth is also fueled by an increased focus on health awareness and preventive care. Mobile hospitals reach underserved populations, offering health screenings, vaccination drives, and educational programs that significantly impact public health outcomes. Furthermore, the regulatory landscape is adapting to more favorably support mobile healthcare solutions, ensuring compliance with health standards and enhancing patient safety.
Recent developments underscore the market’s dynamic nature. In November 2023, the World Health Organization and Siemens Healthineers announced a collaboration to deploy mobile hospitals in ten developing countries by 2025, aiming to improve healthcare access in regions with limited medical facilities. Additionally, Inmarsat and eHealth Africa launched a telemedicine platform designed for remote diagnosis and treatment in mobile hospitals, enhancing care in remote areas. Moreover, Royal Philips expanded its mobile imaging portfolio, which includes portable X-ray and ultrasound devices tailored for use in various settings, thereby facilitating immediate patient diagnosis and treatment. These advancements are pivotal in shaping the future of mobile healthcare, emphasizing innovation and strategic collaborations to enhance global health outcomes.
Key Takeaways
- The Global Mobile Hospitals Market is projected to grow to USD 62.6 billion by 2033 from USD 22.6 billion in 2023.
- This market anticipates a 12% Compound Annual Growth Rate (CAGR) from 2023 to 2033.
- In 2023, Accident & Emergency Care Facilities were the largest segment, claiming over 27.5% market share.
- Therapy/Treatment services led the market in 2023, making up more than 29.8% of the total market share.
- North America held a dominant position in 2023, with a market value of USD 8.3 billion, representing 39.8% of the market.
- The Asia Pacific region shows substantial growth prospects, particularly in India and China, indicating its emerging market presence.
Mobile Hospitals Statistics
- 60% of the global population uses mobile devices to access healthcare services, making mobile hospitals essential for patient-centered care.
- Survey Overview: A comprehensive survey covered 364 general hospitals regarding the implementation of mobile-based Patient Health Record (m-PHR) systems.
- Hospital Types Involved: Among the surveyed institutions, 43 are tertiary hospitals, recognized for specialized medical services across regions.
- m-PHR System Implementation: Approximately 27.7% of these hospitals, totaling 101, have successfully adopted the m-PHR system.
- Geographical Distribution: Of the hospitals analyzed, 56% are situated in Seoul and other large metropolitan areas.
- Ownership Structure: A significant majority, 75.8%, of the hospitals are privately owned.
- Operational Tenure: The average operational duration of these hospitals is 33 years.
- Hospital Classification: About 40% of the surveyed hospitals are classified as tertiary.
- Systemic Affiliation: Nearly 78% are part of broader multi-hospital systems.
- Adoption Rates by Type: Tertiary general hospitals show a high adoption rate of 61.9%, whereas general hospitals with 300+ beds have a 22.6% adoption rate.
- Setup Time: Mobile hospitals typically require 48 to 72 hours to become fully operational.
- Patient Capacity: These facilities can accommodate and treat between 200 and 300 patients daily.
- COVID-19 Adaptation: To manage increased patient loads during the pandemic, mobile hospitals expanded their operations by 20%.
- Operational Lifespan: With regular maintenance, mobile hospitals can remain operational for 10 to 15 years.
- Global Deployment: These units have been deployed in over 50 countries to provide critical care during disasters or conflicts.
- Zealand University Hospital in Denmark has acquired 35 mobile robots to enhance its operational capabilities.
- A standard mobile hospital typically employs between 50 and 100 medical personnel, including doctors, nurses, and support staff.
- Mobile hospitals are designed to be rapidly deployed, becoming operational within 24 to 48 hours during emergency scenarios.
Emerging Trends
- AI-Driven Diagnostics: The integration of artificial intelligence (AI) into mobile health applications marks a significant step forward in diagnostic capabilities. AI algorithms are becoming increasingly adept at analyzing real-time data and medical images with remarkable precision. This advancement not only accelerates the diagnostic process but also enhances the accuracy of patient outcomes. By leveraging AI, healthcare providers can detect complex conditions earlier and with greater confidence, leading to improved treatment plans and better health management.
- Augmented Reality (AR) in Healthcare: Augmented reality is set to revolutionize the healthcare field by enhancing patient engagement and educational experiences. AR technology provides interactive, three-dimensional simulations that can be used for both patient education and professional medical training. These realistic simulations help patients better understand their conditions and treatments, thereby improving their engagement with the healthcare process. For healthcare professionals, AR serves as a valuable tool in training scenarios, offering hands-on experience without the risks associated with real-life procedures.
- Advanced Wearables: The development of advanced wearable technology continues to play a crucial role in health monitoring. These devices are designed to track a wide range of health metrics, such as vital signs, activity levels, and sleep patterns. The data collected by wearables is integral to developing personalized and preventive healthcare plans. With real-time health monitoring, both patients and healthcare providers can promptly address potential health issues before they escalate, supporting a proactive approach to health management.
- Virtual Consultations: Virtual consultation technology is enhancing the accessibility of healthcare, particularly for individuals with mobility limitations or those residing in remote areas. Through mobile health apps, patients can now consult with healthcare professionals from the comfort of their homes. This convenience ensures that more people can access quality healthcare without the need to travel, reducing both time and financial constraints associated with traditional in-person visits.
- Personalized Wellness Programs: Personalization is becoming a key trend in healthcare, with mobile apps increasingly able to tailor wellness plans based on individual health data. These personalized programs consider various factors such as medical history, lifestyle choices, and genetic predispositions to create customized health and wellness plans. This approach empowers individuals to take an active role in managing their health, with tailored recommendations that enhance their overall well-being.
Use Cases
- Disaster Response: Mobile hospitals are vital in disaster-stricken regions where traditional medical facilities might be damaged or inaccessible. They provide essential medical services ranging from emergency care to surgical interventions, ensuring that victims receive immediate and effective medical treatment. The ability to quickly establish these mobile units close to disaster sites means that first responders can save more lives by reducing the time between injury and treatment.
- Rural Healthcare Delivery: In rural areas where conventional healthcare infrastructure is sparse or non-existent, mobile hospitals are a critical resource. They bring a wide range of medical services directly to remote communities, from routine health screenings to more complex procedures. This accessibility helps to improve health outcomes by providing timely medical attention that would otherwise require extensive travel to urban centers, thereby removing significant barriers to healthcare access for rural populations.
- Military Applications: Mobile hospitals are indispensable in military contexts, particularly in conflict zones or during field operations. They provide the armed forces with the capability to treat injuries and illnesses on-site, which is crucial for maintaining troop health and readiness. The flexibility and mobility of these units allow for rapid deployment to various locations, ensuring that medical care is available wherever the military operates, even in the most challenging environments.
- Outbreak Containment: During epidemics or pandemics, mobile hospitals are crucial for containing infectious diseases. They can be quickly set up to create isolated treatment areas that help prevent the spread of disease. These units are equipped to provide both diagnostic services and intensive care treatment, which is vital for managing high-risk patients and reducing mortality rates. The strategic deployment of mobile hospitals during health crises can significantly impact public health outcomes by localizing treatment and reducing the load on permanent healthcare facilities.
- Event Healthcare Services: At large public events such as festivals, sports competitions, or concerts, mobile hospitals provide essential medical services on-site. This accessibility ensures that medical emergencies are handled promptly and efficiently, enhancing safety and medical responsiveness. Whether it’s treating minor injuries or responding to more serious health incidents, mobile hospitals help to ensure that event attendees receive immediate care, minimizing potential health risks associated with large crowd gatherings.
Conclusion
The Global Mobile Hospitals Market is set to undergo substantial growth, propelled by technological advancements, heightened government funding, and the growing need for accessible healthcare solutions in remote areas. Technological integration such as telemedicine has enhanced the functionality of mobile hospitals, making them essential in areas where traditional healthcare infrastructure is either limited or non-existent. Government initiatives across various regions are also playing a pivotal role in expanding these services to underserved populations, further driving market growth.
However, challenges such as limited awareness and the shortage of skilled healthcare professionals are significant hurdles. Despite these challenges, the market outlook remains positive with opportunities particularly ripe in emerging economies where healthcare infrastructure is still developing. Innovations in mobile healthcare facilities are expected to continue, focusing on improving accessibility and the effectiveness of medical services provided in disparate conditions.
Discuss your needs with our analyst
Please share your requirements with more details so our analyst can check if they can solve your problem(s)



