Introduction
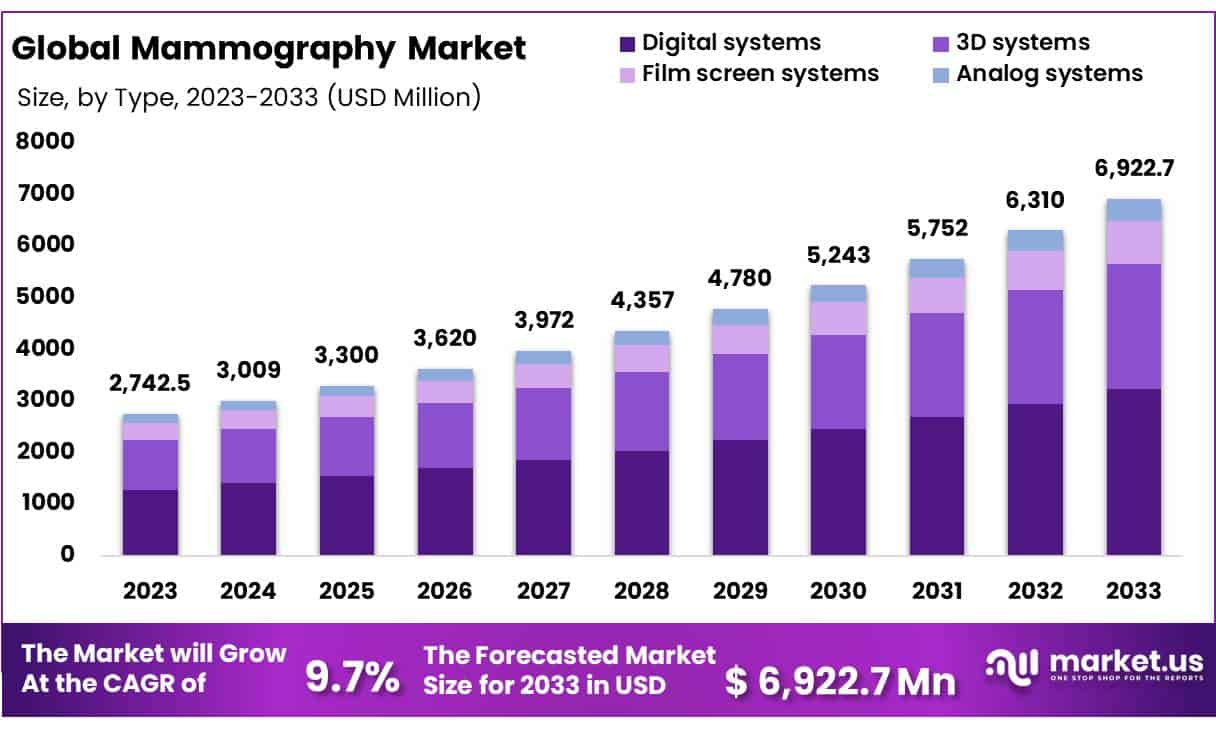
Global Mammography Market size is expected to be worth around USD 6,922.7 Million by 2033 from USD 2,742.5 Million in 2023, growing at a CAGR of 9.7% during the forecast period from 2024 to 2033.The mammography market is experiencing significant growth, primarily driven by advancements in imaging technology and increased awareness of early breast cancer detection.
Leading health organizations like the U.S. Preventive Services Task Force have recently updated their guidelines, recommending that routine mammograms start at age 40 instead of 50. This change reflects rising breast cancer rates among younger women and aims to improve early detection and treatment outcomes. The market is also seeing growth due to the introduction of 3D mammography, which provides more detailed imaging and reduces false positives. These developments highlight the critical role mammography plays in reducing breast cancer mortality rates through earlier diagnosis and intervention.
Despite these advancements, the mammography market faces challenges such as disparities in access to screening services, particularly among underserved populations. High costs of advanced mammography technologies can also limit accessibility in low-income regions, exacerbating healthcare inequities. Additionally, concerns about overdiagnosis and the psychological impact of false positives remain barriers to broader acceptance. Addressing these challenges requires strategic efforts from healthcare providers and policymakers to ensure equitable access and patient education about the benefits and limitations of mammography. Continuous improvements in technology and increased funding for screening programs are essential to overcome these obstacles and enhance patient outcomes.
Key Takeaways
- Market Size: Global Mammography Market size is expected to be worth around USD 6,922.7 Million by 2033 from USD 2,742.5 Million in 2023.
- Market Growth: Global Mammography Market is growing at a CAGR of 9.7% during the forecast period from 2024 to 2033.
- Product Type Analysis: Digital systems hold a 46.8% market share in the mammography market in 2023, reflecting their widespread adoption in medical imaging.
- Technology Analysis: Digital mammography dominates the market with an 80.9% share in 2023, underscoring its importance in modern breast cancer screening.
- End-Use Analysis: Mammography devices used in hospital settings account for 76.2% of the market share, highlighting the preference for hospital-based screening facilities.
- Regional Analysis: North America is expected to hold the largest market share at 43.5%, with revenues reaching USD 1,192.9 million, driven by advanced healthcare infrastructure.
- Rising Incidence of Breast Cancer: The growth of the mammography market is directly linked to increasing global breast cancer incidence rates and the consequent need for early detection and diagnosis.
- Heightening Awareness: Campaigns and government initiatives promoting breast screenings have effectively raised public and patient awareness, contributing to market expansion.
Mammography Statistics
- Starting Age for Screening: The U.S. Preventive Services Task Force updated guidelines in May 2023 to recommend starting regular mammograms at age 40, down from age 50, due to an average annual increase of 2% in breast cancer incidence among women aged 40 to 49 from 2015 to 2019.
- Breast Density Awareness: Approximately 50% of women over 40 in the U.S. have dense breast tissue, which can obscure cancer detection on mammograms. The FDA now mandates facilities to inform patients of breast density and recommend additional screening options.
- Mortality Reduction: Early detection of breast cancer via mammography can reduce mortality rates by 20-40% among women aged 40-74, highlighting the importance of regular screenings.
- Impact on Black Women: Black women are twice as likely to die from breast cancer as white women of the same age. Earlier screening could potentially reduce this disparity by improving early detection rates.
- 3D Mammography Adoption: 3D mammography, also known as digital breast tomosynthesis, is gaining adoption, improving cancer detection rates by 15% compared to traditional 2D mammograms, especially in women under 50.
- False Positive Rates: False positives occur in about 11% of women receiving annual 3D mammograms, compared to 7% for those screened biennially, highlighting the need for precision in screening intervals.
- Technology Integration: Digital mammography systems facilitate image sharing and enhance diagnostic accuracy, with computer-aided detection tools improving identification of abnormalities.
- Mobile Mammography Units: Mobile units are crucial in increasing access to mammography services, particularly in rural and underserved areas, ensuring that more women receive screenings regardless of location.
- Breast Cancer Risk Factors: Dense breast tissue is a risk factor for breast cancer, and women with dense breasts may benefit from additional imaging such as MRI or ultrasound.
- Screening Uptake: Screening uptake varies by demographic, with disparities evident in 3D mammography usage among different racial/ethnic groups.
- Psychological Impact: False positives can cause anxiety and lead to unnecessary biopsies, but most are resolved with follow-up imaging, emphasizing the need for careful communication and support.
- Cost-Effectiveness: Mammograms are considered cost-effective, especially when early detection leads to less aggressive and less costly treatments.
- Genetic Risk Considerations: Women with genetic predispositions, such as BRCA1/2 mutations, are advised to start screenings earlier and undergo more frequent mammograms.
- Screening Frequency: Annual screening is recommended for high-risk groups, while average-risk women can opt for biennial screening after age 55.
- Policy Changes: Changes in screening guidelines are expected to affect millions of women, ensuring better coverage and earlier interventions for breast cancer.
Emerging Trend
- Early Detection of Breast Cancer: Mammography is a cornerstone in the early detection of breast cancer, capable of capturing detailed images of breast tissue to identify abnormalities before they become palpable or symptomatic. Early detection through mammography significantly improves treatment outcomes by allowing for less aggressive treatment options and increasing survival rates. Studies show that early detection can reduce breast cancer mortality by 25-30% among women aged 40 to 70, emphasizing the importance of regular screenings.
- Screening Programs for High-Risk Populations: For high-risk populations, such as women with a family history of breast cancer or genetic predispositions like BRCA1 and BRCA2 mutations, mammography is essential. These groups require more frequent and earlier screenings to catch potential malignancies early. Tailored screening programs are designed to identify cancer at the earliest possible stage, which is crucial for successful intervention and improved survival rates. Genetic counseling and risk assessment are often combined with regular mammographic screenings for comprehensive care.
- Routine Screening for Average-Risk Women: Routine mammograms are recommended for women over 40 to screen for breast cancer. This practice reduces breast cancer mortality by detecting tumors at an early, more treatable stage. Regular screening is a preventive measure that helps in managing healthcare costs by reducing the need for more extensive treatments that are necessary for advanced cancer. Mammography is widely accepted as the standard for regular screening and is supported by many health organizations worldwide.
- Assessment of Breast Abnormalities: When breast abnormalities are detected through physical exams, ultrasounds, or patient-reported symptoms, mammograms are used to evaluate these findings. The detailed imagery provided by mammography helps in diagnosing the nature of these abnormalities, differentiating between benign and malignant growths. This diagnostic capability reduces unnecessary anxiety and enables doctors to decide the appropriate course of action, whether it be further testing, monitoring, or immediate treatment.
- Monitoring After Cancer Treatment: For patients who have undergone breast cancer treatment, mammography is a critical tool for monitoring any recurrence of cancer. Regular post-treatment mammograms help detect any new or recurring tumors early, allowing for timely intervention and treatment adjustments. This monitoring is vital for maintaining remission and improving long-term survival rates, as early detection of recurrence can significantly influence outcomes.
- Guidance for Biopsy Procedures: Stereotactic mammography is used to guide needle biopsies with precision, ensuring accurate sampling of suspicious areas. This technique minimizes the need for more invasive surgical biopsies and allows for a more targeted approach to diagnosing potential malignancies. By providing detailed imagery of the breast tissue, stereotactic mammography increases the accuracy of biopsies and reduces the risk of sampling errors.
- Integration with Digital Technologies: Digital mammography systems enhance image storage and sharing, facilitating consultations between specialists. This integration supports improved diagnostic accuracy and treatment planning by allowing radiologists to manipulate images for better analysis and interpretation. Advanced digital systems also enable the application of computer-aided detection (CAD) tools, which assist in identifying potential areas of concern that may require further investigation.
Use Cases
- Breast Cancer Screening: Mammography is the primary screening tool for breast cancer, helping detect early-stage cancers when treatment is more effective. Regular screenings are recommended for women aged 50 to 74 years to reduce mortality rates.
- Risk Assessment: Mammograms assess breast density, which is a risk factor for breast cancer. Women with dense breast tissue may require additional imaging tests to ensure accurate detection.
- Follow-Up on Symptoms: Mammography is used to evaluate suspicious findings from physical exams or other imaging tests, such as lumps or changes in breast tissue.
- Surveillance in Cancer Survivors: Women previously diagnosed with breast cancer undergo routine mammograms to monitor for any signs of recurrence or new cancers.
- Quality Standards: The Mammography Quality Standards Act (MQSA) ensures that facilities meet high standards for image quality and patient care, improving diagnostic accuracy.
- Digital Mammography: Digital mammography provides clearer images and allows for easier storage and retrieval, which can improve diagnostic capabilities and workflow efficiency.
- 3D Mammography (Tomosynthesis): This advanced technique offers a three-dimensional view of the breast, improving the detection of small tumors and reducing false positives.
- Breast Density Notification: Legislation requires facilities to inform patients about breast density and its implications, encouraging informed discussions about screening options.
Conclusion
The mammography market is set to grow significantly, with expectations to reach USD 6,922.7 million by 2033, driven by technological advancements and increased early detection awareness. The shift to recommending mammograms starting at age 40, along with the adoption of 3D mammography and AI, enhances diagnostic accuracy and reduces mortality rates. However, challenges like disparities in access and high costs of advanced technologies persist. Addressing these issues requires concerted efforts from healthcare providers and policymakers to ensure equitable access and patient education. Continuous technological improvements and increased funding for screening programs are crucial for overcoming these challenges and improving patient outcomes.
Discuss your needs with our analyst
Please share your requirements with more details so our analyst can check if they can solve your problem(s)



