Introduction
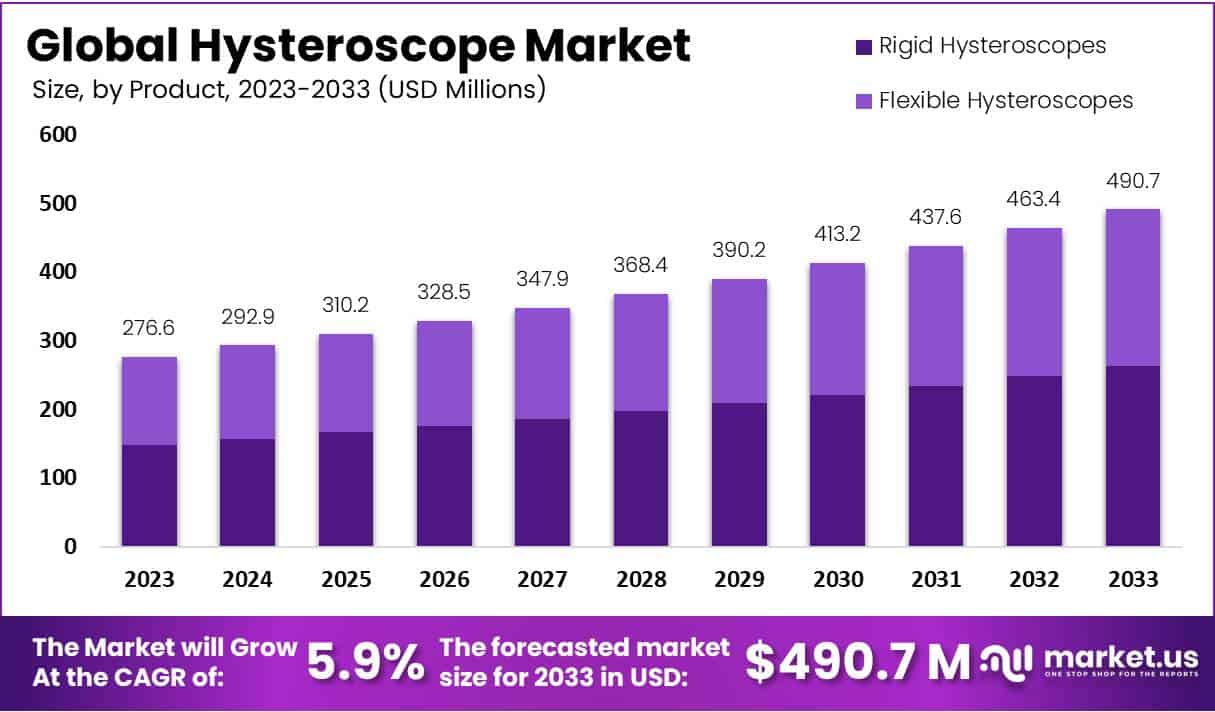
The Hysteroscope Market is poised for substantial growth, projected to escalate from USD 276.6 million in 2023 to approximately USD 490.7 million by 2033. This expansion reflects a steady compound annual growth rate (CAGR) of 5.9% from 2024 to 2033. Driving this growth are technological advancements in minimally invasive procedures, which position hysteroscopy as a favored approach for diagnosing and treating various uterine conditions, including fibroids, polyps, and abnormal bleeding. Typically affecting women aged 30 to 60, these conditions demand efficient and less invasive treatment options.
Hysteroscopy’s integration into fertility treatments further amplifies its significance. Diagnostic hysteroscopy is increasingly utilized to examine the uterine environment prior to in vitro fertilization (IVF), playing a critical role in reproductive healthcare. This procedure aids in detecting and addressing factors that might obstruct embryo implantation, thus enhancing the success rates of fertility treatments. Such diagnostic advancements are vital for patients looking to conceive, reinforcing the procedure’s adoption rate.
Insurance coverage also plays a crucial role in promoting the accessibility and utilization of hysteroscopy. Most insurance plans now cover hysteroscopic procedures when deemed medically necessary, alleviating financial concerns for patients and encouraging them to opt for this safer, less invasive method. This coverage ensures that more patients can afford hysteroscopy, which is often necessary for comprehensive gynecological care.
Technological advancements in hysteroscopic equipment have significantly improved the procedure’s safety and effectiveness. Enhancements in imaging quality and surgical tools not only boost the procedure’s efficacy but also facilitate its execution in outpatient settings without the need for general anesthesia. This shift not only underscores the procedure’s efficiency and cost-effectiveness but also aligns with the broader medical trend towards outpatient care solutions.
Lastly, educational initiatives by healthcare institutions and the availability of specialized training for practitioners enhance the quality and safety of hysteroscopic procedures. These efforts ensure that healthcare providers are proficient in utilizing the latest hysteroscopic technologies and techniques, fostering further growth in the sector. The combined impact of these factors establishes a robust foundation for the ongoing expansion of the hysteroscope market, mirroring the general shift towards minimally invasive medical practices.
Key Takeaways
- The market is projected to reach USD 490.7 million by 2033, growing at a CAGR of 5.9% from 2024.
- Rigid hysteroscopes were the leading product, holding a 53.6% market share in 2023.
- Myomectomy was the leading application with a 38.5% market share in 2023, primarily for treating uterine fibroids.
- Hospitals were the primary end-users, dominating with a 52.6% market share in 2023.
- Market growth is driven by rising gynecological disorders and increased global healthcare spending.
- Challenges include high costs, a shortage of skilled professionals, and concerns over infection control.
- Opportunities for growth include expanding into emerging markets and developing disposable hysteroscopes.
- Trends include a shift to minimally invasive procedures, AI integration, and device customization.
- North America held a leading position in the market with a 40.6% share, valued at USD 112 million in 2023.
- Collaborations in the industry are enhancing innovation and integrating hysteroscopic procedures with telemedicine.
Emerging Trends
- Office-Based Procedures: Hysteroscopy is shifting from hospitals to doctor’s offices. This change eliminates the need for general anesthesia, reducing costs and speeding up recovery. Office-based hysteroscopy is also more convenient for patients, allowing them to return to daily activities quickly. Studies show that around 98.66% of these procedures are successful. This high success rate makes office-based hysteroscopy a preferred choice for many women. Additionally, avoiding hospitalization lowers the risk of infections. Doctors are now recommending this approach for diagnosing and treating conditions like polyps, fibroids, and abnormal bleeding. With improved efficiency, more women can access hysteroscopy without long hospital wait times.
- Advancements in Equipment: Smaller and more flexible hysteroscopes are transforming the procedure. Traditional hysteroscopes were larger, causing discomfort and requiring sedation. Modern versions are designed for a pain-free experience, making the procedure easier for both patients and doctors. These improvements also expand the use of hysteroscopy in diagnosing and treating more conditions. With better imaging and enhanced maneuverability, doctors can detect abnormalities more accurately. The shift toward minimally invasive devices allows real-time evaluation of the uterus with minimal discomfort. As a result, more women are willing to undergo hysteroscopy, leading to early detection of conditions like fibroids, adhesions, and endometrial polyps.
- Enhanced Diagnostic Techniques: Hysteroscopy is now used to check fallopian tube openness. This advancement is crucial for infertility assessments, allowing doctors to determine potential causes of pregnancy challenges. Previously, women needed separate tests for this evaluation. With new hysteroscopic methods, doctors can assess tubal patency in the same procedure, saving time and reducing stress. This technique also improves treatment planning by providing immediate insights into uterine health. As technology evolves, hysteroscopy is becoming a key tool in reproductive health. Women struggling with conception now have access to quicker, more accurate diagnoses, leading to personalized fertility treatments.
- Integration with Fertility Treatments: Hysteroscopy is playing a growing role in fertility treatments. Many women with unexplained infertility may have undiagnosed uterine abnormalities. Hysteroscopy helps detect and treat these issues, improving the chances of successful conception. It is now widely used before in-vitro fertilization (IVF) to optimize the uterine environment. Studies suggest that correcting uterine abnormalities can increase pregnancy success rates. This procedure is also beneficial for women with repeated miscarriages, as it helps identify potential causes. With rising infertility cases, hysteroscopy is becoming an essential tool in assisted reproductive technologies. Doctors recommend it to ensure a healthy uterus for implantation and pregnancy.
Use Cases
- Investigating Abnormal Uterine Bleeding: Hysteroscopy is a key procedure for diagnosing unusual uterine bleeding. It provides a clear view of the uterine lining, helping doctors identify potential causes like polyps, fibroids, or abnormal tissue growth. This method is minimally invasive and allows real-time assessment. It is often recommended for women experiencing heavy, prolonged, or irregular menstrual cycles. Compared to traditional diagnostic methods, hysteroscopy provides more accurate results. In some cases, doctors can treat the condition immediately, avoiding the need for multiple procedures. This approach improves patient outcomes and reduces discomfort. By addressing the root cause early, hysteroscopy helps prevent complications and enhances overall reproductive health.
- Removing Uterine Polyps and Fibroids: Hysteroscopy effectively removes uterine polyps and fibroids, which are common non-cancerous growths. These growths can lead to symptoms like heavy bleeding, pain, and fertility issues. During the procedure, doctors use a thin, lighted tube to locate and remove these abnormalities. In a study of 3,000 office hysteroscopies, 37.8% were operative, meaning treatment was performed during the same session. This eliminates the need for additional surgeries, making it a convenient and efficient solution. Many women experience immediate symptom relief after polyp or fibroid removal. Hysteroscopy is a safer alternative to traditional surgery and has a quicker recovery time. It also lowers the risk of complications and improves overall uterine health.
- Assessing and Treating Infertility: Hysteroscopy plays a crucial role in fertility assessments. It helps doctors detect and correct uterine abnormalities that may prevent pregnancy. Common issues include adhesions, polyps, or a septate uterus, all of which can interfere with embryo implantation. By addressing these problems, hysteroscopy improves fertility outcomes. The procedure is often used before in vitro fertilization (IVF) to optimize uterine conditions. Many studies highlight its benefits in increasing pregnancy success rates. Unlike other diagnostic tools, hysteroscopy allows direct visualization of the uterus, ensuring more precise treatment. Women experiencing recurrent miscarriages or failed IVF cycles may benefit from this procedure. It provides both diagnosis and treatment in a single session.
- Diagnosing and Managing Chronic Endometritis: Hysteroscopy is an effective tool for detecting chronic endometritis, a condition caused by persistent inflammation of the uterine lining. This condition often goes unnoticed due to mild or absent symptoms. However, it can significantly impact fertility, leading to implantation failure in assisted reproductive treatments. Hysteroscopy allows doctors to take a small tissue sample for further analysis. If chronic endometritis is confirmed, targeted antibiotic therapy can be prescribed. Studies show that treating this condition increases pregnancy rates in women struggling with infertility. Early diagnosis and treatment can prevent long-term complications. Hysteroscopy offers a reliable and efficient way to manage this hidden but impactful condition.
- Evaluating Fallopian Tube Patency: Hysteroscopy is used to check if the fallopian tubes are open, a critical factor in fertility. Blocked fallopian tubes can prevent pregnancy by stopping the egg from reaching the uterus. Traditionally, an X-ray or ultrasound was used for this assessment, but hysteroscopy provides a more accurate and direct approach. A contrast fluid is introduced into the tubes, and its movement is observed. If a blockage is found, additional treatment options can be explored. This procedure is safe, well-tolerated, and provides immediate results. Many women prefer hysteroscopy over other methods due to its minimal discomfort and quick recovery time. It offers a comprehensive evaluation of reproductive health.
Regional Analysis
In 2023, North America led the global Hysteroscope market, holding over a 40.6% share. The market value reached USD 112 million, highlighting strong regional growth. Several factors fueled this dominance, including advanced healthcare infrastructure, increased awareness of gynecological disorders, and rising investments in research. The demand for Hysteroscopes surged due to improved diagnostic technologies and better access to healthcare services. These trends positioned North America as a key region for market expansion, setting a high standard for adoption and innovation.
The presence of well-equipped healthcare facilities played a major role in driving market growth. North America’s advanced medical infrastructure enabled quicker adoption of Hysteroscopes for diagnosis and treatment. A rising prevalence of gynecological disorders further increased demand for these devices. Additionally, a proactive approach to women’s health led to higher screening rates. With a growing focus on early diagnosis, hospitals and clinics integrated modern hysteroscopy techniques, improving patient outcomes and expanding the market.
Key industry players strengthened North America’s market leadership through product innovation and strategic partnerships. Major companies focused on developing advanced Hysteroscopes with improved imaging and minimally invasive capabilities. Collaborations between healthcare institutions and manufacturers enhanced clinical efficiency. These efforts facilitated the seamless integration of Hysteroscopes into gynecological procedures. Ongoing research and development further expanded the scope of applications, ensuring continuous market growth.
Government initiatives played a crucial role in boosting market adoption. Awareness programs and public health campaigns emphasized early detection of gynecological conditions. Funding for research and improved reimbursement policies encouraged healthcare providers to use advanced Hysteroscopes. Screening programs increased patient access to diagnostic procedures, supporting market expansion. These factors, combined with technological advancements, reinforced North America’s dominant position in the global Hysteroscope market.
Conclusion
The Hysteroscope Market is set for strong growth, driven by technological advancements, rising awareness of gynecological conditions, and increasing demand for minimally invasive procedures. The adoption of hysteroscopy in fertility treatments and diagnostic applications further enhances its importance. Improved imaging and flexible devices make the procedure safer, more effective, and widely accessible. Insurance coverage and outpatient care trends support market expansion, making hysteroscopy a preferred choice for many women. The market benefits from strong healthcare infrastructure, ongoing research, and strategic collaborations. With continuous innovation and growing applications in gynecology, hysteroscopy is expected to remain a key tool for diagnosis and treatment, contributing to better patient outcomes worldwide.
Discuss your needs with our analyst
Please share your requirements with more details so our analyst can check if they can solve your problem(s)



