Table of Contents
Overview
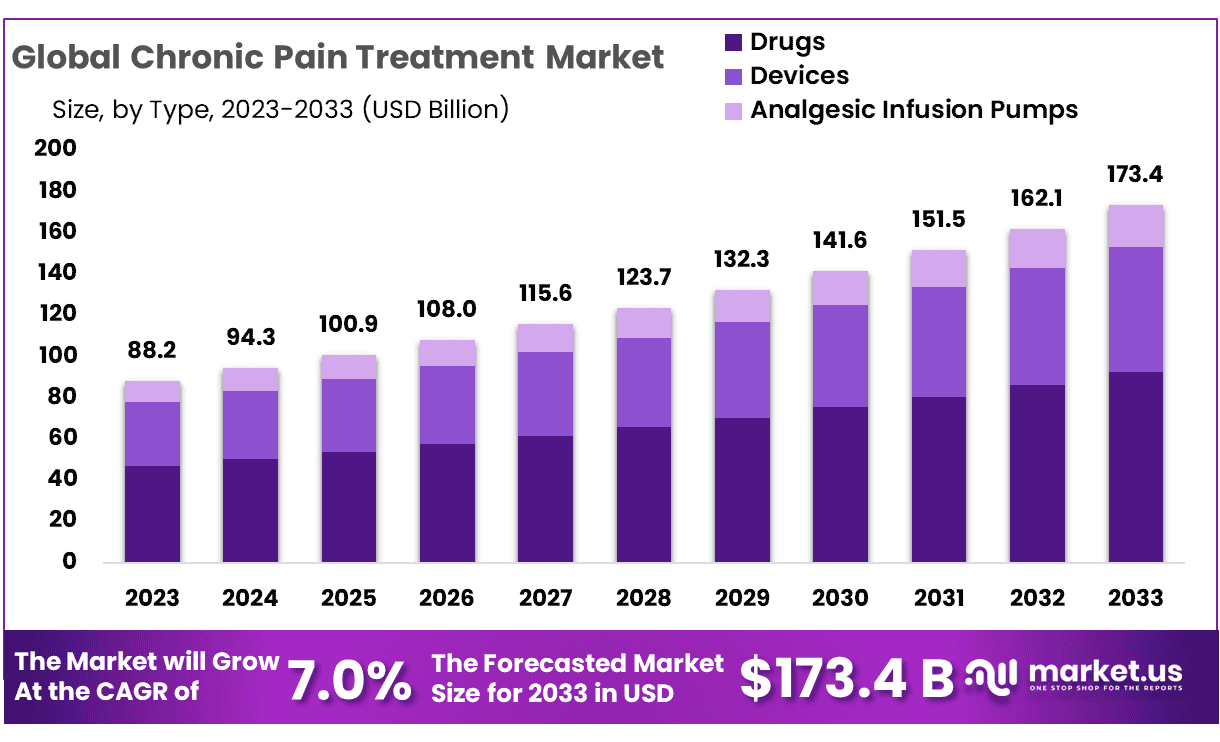
New York, NY – Jan 21, 2026 – The Global Chronic Pain Treatment Market size is expected to be worth around USD 173.4 Billion by 2033 from USD 88.2 Billion in 2023, growing at a CAGR of 7.0% during the forecast period from 2024 to 2033.
Chronic pain continues to be a significant public health concern, affecting millions of individuals worldwide and placing sustained pressure on healthcare systems. In response, structured and evidence-based approaches to chronic pain treatment are increasingly being emphasized to improve patient outcomes and quality of life.
The basic foundation of chronic pain treatment is built on a multidisciplinary model. It is widely recognized that effective management cannot rely on a single intervention. Instead, treatment strategies are designed to address physical, psychological, and functional dimensions of pain. This integrated framework supports long-term symptom control rather than short-term relief alone.
Pharmacological therapy remains a core component of treatment and is typically administered in carefully monitored doses to reduce pain intensity and inflammation. At the same time, non-pharmacological interventions such as physical therapy are incorporated to restore mobility, strengthen muscles, and improve daily functioning. These therapies are structured to reduce dependency on medication over time.
Behavioral and cognitive-based therapies also play an essential role. Chronic pain is closely linked with stress, anxiety, and sleep disturbances, and these factors are addressed through guided psychological support and patient education. Lifestyle modifications, including exercise planning and ergonomic adjustments, are increasingly integrated into care pathways.
The adoption of a comprehensive treatment foundation reflects a growing shift toward patient-centered care. This approach is expected to support sustainable pain management outcomes and aligns with broader trends toward holistic and value-based healthcare delivery.
For healthcare providers and stakeholders, this foundational model represents a structured and scalable framework for addressing the long-term challenges of chronic pain management.
Key Takeaways
- Market Size: The chronic pain treatment market is projected to reach approximately USD 173.4 billion by 2033, increasing from USD 88.2 billion in 2023.
- Market Growth: Market expansion is expected to occur at a compound annual growth rate (CAGR) of 7.0% over the forecast period from 2024 to 2033.
- Type Analysis: Drug-based therapies remain the leading treatment category, accounting for 53.2% of the total market share.
- Indication Analysis: Neuropathic pain represents the largest indication segment, capturing 31.6% of the chronic pain treatment market.
- End User Analysis: Hospitals constitute the primary end-user segment, holding a dominant 61.2% market share.
- Regional Analysis: North America is expected to maintain its leading position, contributing 46.5% of the global market share and generating approximately USD 41 billion in chronic pain treatment revenues.
Indication Analysis of Chronic Pain Treatment
- Cancer Pain: Cancer-related pain is primarily driven by tumor progression, adverse effects of treatment, and associated complications. The prevalence differs by cancer type and disease stage. Clinical evidence indicates that pain is experienced by approximately 30%–50% of cancer patients, rising sharply to 70%–90% in advanced stages. Effective pain management is considered essential for improving patient comfort, functional ability, and overall quality of life.
- Arthritic Pain: Arthritic pain results from chronic joint inflammation and structural degeneration, most commonly associated with osteoarthritis and rheumatoid arthritis. According to data from the Centers for Disease Control and Prevention (CDC), nearly 24% of adults in the United States are affected by arthritis, with a substantial proportion experiencing persistent pain that restricts mobility and daily functioning.
- Acute Appendicitis: Acute appendicitis is characterized by sudden inflammation of the appendix, leading to intense abdominal pain. Although the condition requires immediate surgical treatment, it is generally resolved following intervention and does not typically progress to chronic pain. As a result, appendicitis is not a key focus within chronic pain treatment markets.
- Neuropathic Pain: Neuropathic pain arises from damage or dysfunction of the nervous system, often linked to diabetes, infections, traumatic injuries, or neurological disorders. Epidemiological studies estimate that neuropathic pain affects approximately 7%–10% of the global population. This condition is frequently associated with long-term disability and often necessitates specialized and targeted treatment approaches.
- Post-Operative Pain: Post-operative pain is a common outcome following surgical procedures and is usually acute. However, inadequate pain control may lead to chronic post-surgical pain (CPSP). Clinical studies indicate that CPSP develops in roughly 10%–50% of patients, depending on the type of surgery performed and individual patient risk factors.
- Fibromyalgia: Fibromyalgia is a chronic disorder marked by widespread musculoskeletal pain, fatigue, and localized tenderness. Estimates from the National Institutes of Health (NIH) suggest that fibromyalgia affects around 4 million adults in the United States, representing approximately 2% of the adult population. The condition is observed more frequently in women and is associated with significant long-term pain burden.
- Migraine: Migraine is a neurological condition characterized by recurrent, severe headaches, often accompanied by nausea, photophobia, and phonophobia. The CDC reports that migraines affect about 15% of U.S. adults, with higher prevalence among women. Migraines are a major contributor to chronic pain and work-related disability.
- Bone Fracture Pain: Bone fractures typically cause acute pain during the healing phase. However, a subset of patients may develop chronic pain due to delayed healing, nerve involvement, or other complications. Some studies indicate that up to 20% of individuals experience persistent pain following a fracture, highlighting the need for effective post-injury pain management.
- Muscle Sprain and Strain: Muscle sprains and strains are among the most common causes of musculoskeletal pain and are generally acute in nature. While most cases resolve with appropriate treatment, improper or delayed management can result in prolonged or chronic pain. Reliable data on the prevalence of chronic pain from these injuries remain limited.
Regional Analysis
The global chronic pain treatment market is segmented into six key regions: North America, Western Europe, Eastern Europe, Asia Pacific (APAC), Latin America, and the Middle East & Africa. Among these, North America is expected to retain a leading position, accounting for an estimated 46.5% of the global market share and generating approximately USD 41 billion in revenue from chronic pain treatments.
This regional dominance is primarily driven by the strong presence of major pharmaceutical companies, extensive drug development activities, and a well-established healthcare infrastructure. In addition, sustained investments in research and development, along with strategic initiatives by industry leaders, have accelerated advancements in chronic pain therapeutics, thereby reinforcing North America’s leadership position in the global market.
Emerging Trends
- Neuromodulation Techniques: Advances in neuromodulation, including spinal cord stimulation (SCS), are expanding therapeutic options for chronic pain management. These techniques modulate pain signaling through targeted electrical stimulation and have shown effectiveness in conditions such as chronic back pain and neuropathic pain.
- Mindfulness-Based Interventions: Mindfulness-based practices, particularly meditation, are increasingly recognized as supportive therapies for chronic pain. Clinical studies suggest that regular mindfulness practice can reduce pain perception, enhance emotional resilience, and improve overall quality of life.
- Dietary Interventions: Growing evidence indicates that dietary patterns rich in vegetables, fruits, whole grains, lean proteins, and dairy products may contribute to pain reduction. The benefits are often attributed to anti-inflammatory effects and improved metabolic health.
- Non-Opioid Pharmacological Innovations: The development of non-opioid analgesics is gaining momentum due to concerns surrounding opioid dependence. Novel drug classes, such as monoacylglycerol lipase (MAGL) inhibitors, have demonstrated promising analgesic effects in early-stage research while minimizing addiction risk.
Key Use Cases
- Spinal Cord Stimulation (SCS): SCS has been widely adopted for the management of chronic back and limb pain. Clinical studies report meaningful improvements in pain intensity and quality of life, with approximately 85% of treated patients experiencing measurable clinical benefits.
- Mindfulness Meditation: In clinical practice, patients engaging in daily mindfulness meditation sessions of approximately 20 minutes have reported reductions in pain severity and discomfort. These findings support its role as a complementary, non-pharmacological intervention.
- Dietary Modification: Adherence to balanced, nutrient-dense dietary guidelines has been associated with lower chronic pain levels, particularly among female populations. This underscores the potential role of nutrition as an adjunct strategy in pain management.
- Non-Opioid Medications: Emerging non-opioid therapies targeting specific pain pathways are providing alternative treatment options. For example, MAGL inhibitors have shown encouraging results in preclinical models, offering analgesic efficacy without the addictive profile of opioids.
Frequently Asked Questions on Chronic Pain Treatment
- What are the major treatment types used in chronic pain management?
Major treatment types include prescription medications such as opioids, NSAIDs, antidepressants, and anticonvulsants. These therapies are often supported by physiotherapy, behavioral therapy, and advanced pain intervention procedures for effective long-term management. - What are the key factors driving chronic pain treatment market growth?
Market growth is driven by rising incidences of chronic disorders, an expanding geriatric population, growing awareness of pain management, and sustained investments in pharmaceutical research and development focused on innovative pain therapies. - Which indication segment dominates the chronic pain treatment market?
Neuropathic pain dominates the market due to its complex clinical nature and high treatment demand. Increased diagnosis rates and the need for long-term therapeutic approaches have strengthened its share within the overall chronic pain treatment landscape. - Who are the main end users of chronic pain treatment solutions?
Hospitals represent the leading end-user segment, benefiting from advanced medical infrastructure, specialized pain management departments, and multidisciplinary treatment capabilities that support comprehensive chronic pain diagnosis and long-term patient care. - Which region holds the largest share in the chronic pain treatment market?
North America holds the largest market share, supported by a well-established pharmaceutical industry, high healthcare expenditure, favorable reimbursement policies, and continuous innovation in chronic pain therapeutics. - What future trends are shaping the chronic pain treatment market?
Future trends include increased adoption of non-opioid therapies, development of personalized pain management solutions, integration of digital health tools, and growing focus on minimally invasive procedures to improve treatment outcomes and patient safety.
Conclusion
Chronic pain treatment is increasingly guided by structured, multidisciplinary and patient-centered care models that address physical, psychological, and functional dimensions of pain. Market growth is being supported by rising chronic disease prevalence, aging populations, and continuous innovation in both pharmacological and non-pharmacological therapies.
Drug-based treatments continue to dominate, while neuropathic pain remains the leading indication due to its complexity and long-term management needs. North America retains market leadership, supported by strong healthcare infrastructure and research activity. Emerging trends such as neuromodulation, non-opioid therapies, mindfulness, and dietary interventions are expected to strengthen sustainable and holistic pain management outcomes.
Discuss your needs with our analyst
Please share your requirements with more details so our analyst can check if they can solve your problem(s)



