Table of Contents
Overview
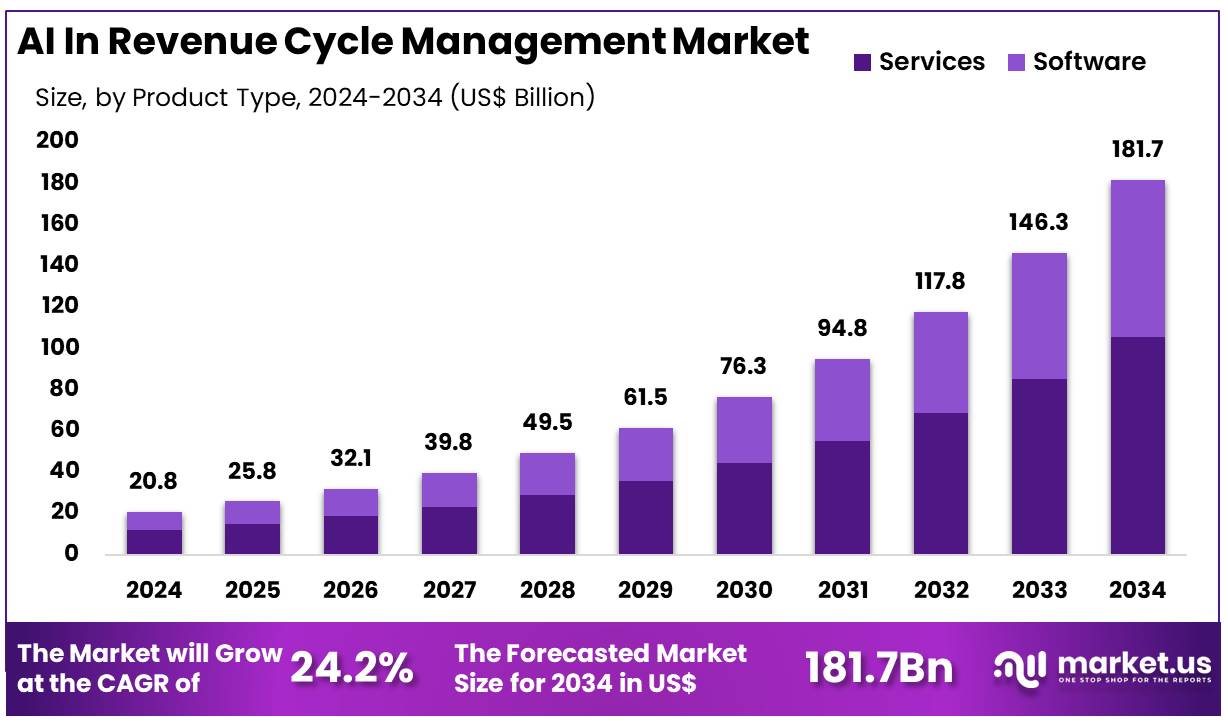
New York, NY – Dec 11, 2025 – Global AI In Revenue Cycle Management Market size is expected to be worth around US$ 181.7 Billion by 2034 from US$ 20.8 Billion in 2024, growing at a CAGR of 24.2% during the forecast period 2025 to 2034. In 2024, North America led the market, achieving over 48.1% share with a revenue of US$ 10.0 Billion.
The adoption of artificial intelligence (AI) in Revenue Cycle Management (RCM) is being recognized as a key driver of operational improvement across healthcare organizations. The deployment of advanced algorithms has been associated with enhanced accuracy in claims processing, accelerated reimbursements, and reduced administrative burdens. The increasing complexity of billing workflows has created the need for intelligent solutions, and AI-driven platforms are being utilized to automate routine tasks, identify coding discrepancies, and predict denial risks.
Significant progress has been observed in front-end functions, where AI tools have been used to verify patient eligibility, estimate out-of-pocket expenses, and streamline prior authorization procedures. The improvement of these processes has contributed to fewer claim errors and stronger financial visibility for providers. In mid-cycle operations, AI has supported clinical documentation integrity by extracting key information from medical records and aligning it with compliant coding standards. This has increased documentation accuracy and strengthened revenue capture.
Back-end functions have also benefited from AI-enabled analytics, which are being used to monitor payment patterns, prioritize accounts, and forecast cash flow. Healthcare organizations have reported measurable gains in staff productivity, as manual workloads have been reduced and high-value tasks have been prioritized.
The market outlook for AI in RCM remains positive, as growing healthcare digitization and the demand for cost-efficient operations continue to support adoption. The advancement of machine learning and automation technologies is expected to strengthen financial performance across provider networks, while ensuring higher transparency and improved patient experience.
Key Takeaways
- The global market for AI in revenue cycle management generated US$ 20.8 billion in 2024, supported by a 24.2% CAGR, and is projected to reach US$ 181.7 billion by 2034.
- The services segment accounted for the leading share of 58.2% within the product type category in 2024.
The integrated technology segment held a dominant position with a 63.5% share. - Within applications, claims management emerged as the leading segment, capturing 25.5% of total revenue.
The web-based delivery mode accounted for the largest share at 54.1%. - Among end users, hospitals represented the primary segment with a 45.3% share.
- North America led the global market with a 48.1% share in 2024.
Regional Analysis
North America accounted for the largest share of 48.1% in 2024, driven by the rising need among healthcare providers and payers to improve efficiency, reduce administrative workloads, and strengthen financial performance. Increasing complexities in billing, coding, and claims processing, combined with escalating operational costs, have accelerated the adoption of AI-enabled solutions. Artificial intelligence supports denial prevention, automated coding, and intelligent claims processing, addressing major administrative challenges.
Major organizations such as UnitedHealth Group continue to invest in digital transformation, with Optum reporting revenues of US$253 billion in 2024, a significant rise from US$64.97 billion in 2023. Government bodies also emphasize digital advancement. The US Department of Health and Human Services highlights AI’s role in administrative forecasting and payment planning, while the Centers for Medicare & Medicaid Services processes over one billion claims annually, underscoring the need for advanced automation.
The Asia Pacific region is projected to grow at the fastest CAGR due to strong digitalization initiatives, demand for cost-efficient administration, and supportive government policies. India’s ABDM has created more than 730 million digital health accounts, and Australia has committed over US$1 billion to strengthen digital health infrastructure. Growing healthcare networks, including IHH Healthcare’s 16% revenue rise to RM24.4 billion, further support AI adoption in financial operations.
Segmentation Analysis
The services segment, holding a 58.2% share, continues to lead the AI in RCM market due to increasing demand for specialized capabilities that streamline revenue cycle workflows. AI-enabled service offerings support hospitals and clinics in billing, coding, claims processing, and analytical functions. Error reduction, faster reimbursement cycles, and improved compliance drive adoption. Growing use of machine learning for denial prediction, eligibility verification, and automated coding further strengthens segment growth as cost efficiency remains a strategic priority.
The integrated technology segment, accounting for 63.5% of the market, is expanding as healthcare organizations prefer unified systems capable of managing claims, billing, coding, and eligibility verification through a single platform. These integrated AI solutions enhance data transparency, reduce manual workloads, and optimize workflow performance. Their strong compatibility with Electronic Health Record (EHR) and Electronic Medical Record (EMR) systems remains a significant contributor to adoption. Real-time analytics and improved interoperability continue to position integrated platforms for long-term dominance.
The claims management segment, representing 25.5% of AI application share, is driven by complexities in billing workflows, rising denial rates, and evolving regulatory requirements. AI tools support automation across claim creation, submission, tracking, and follow-up processes. They reduce human error, improve compliance, and use predictive analytics to identify high-risk claims. These capabilities enable corrective actions that increase success rates. As reimbursement pressures intensify, AI-driven claims management is expected to retain its importance for providers.
The web-based delivery mode, capturing 54.1% of the market, is favored for its scalability, flexibility, and remote accessibility. These platforms enable collaborative operations without significant infrastructure investments and integrate effectively with hospital information systems and EHRs. Their lower maintenance needs and cloud storage advantages further strengthen provider adoption. Increasing attention to security and the rise of remote administrative workflows support sustained dominance of web-based AI tools.
The hospital end-user segment, with a 45.3% share, leads adoption due to the need to manage large volumes of complex billing and enhance financial performance. AI-enabled automation supports coding accuracy, billing efficiency, and streamlined claims management. Rising patient loads and intricate payer requirements increase demand for solutions capable of processing significant data volumes. Regulatory compliance requirements also reinforce adoption, positioning AI-driven RCM tools as essential components of hospital digital transformation strategies.
Use Cases
- Automated Medical Coding: Automated medical coding uses AI to scan clinical documentation and assign precise codes instantly. Accuracy improves, billing cycles accelerate, and compliance is maintained. Reduced manual work and fewer coding errors support faster reimbursements, cost savings, and a smoother revenue cycle for healthcare organizations.
- Claim Scrubbing and Error Detection: AI-driven claim scrubbing identifies coding errors, missing data, and compliance issues before submission. This reduces rejections, speeds insurer approval, and minimizes manual reviews. Higher claim accuracy strengthens cash flow, increases processing efficiency, and supports more dependable revenue cycle performance across healthcare settings.
- Denial Management: AI analyzes denied claims to detect recurring issues, recommend corrective actions, and prevent future denials. Prioritization of high-value recoveries improves resolution speed and revenue retention. Continuous learning reduces staff workload, enhances financial stability, and strengthens denial management effectiveness over time.
- Patient Billing and Payment Reminders: AI automates patient billing, sends personalized reminders, and manages online payments or flexible plans. Timely notifications improve payment compliance, reduce outstanding balances, and increase patient satisfaction. Automated workflows lower administrative burdens and support stronger, more predictable revenue generation for healthcare providers.
- Insurance Eligibility Verification: AI performs real-time insurance verification by linking directly to payer databases. Eligibility issues are prevented, cost estimates become more accurate, and patient transparency improves. Reduced manual checks minimize delays, strengthen reimbursement reliability, and support a more efficient revenue cycle process.
- Revenue Forecasting: AI-powered forecasting evaluates historical payments, seasonal trends, and volume patterns to predict future revenue. Improved financial planning, resource allocation, and risk mitigation strengthen organizational stability. Actionable insights support strategic decisions, helping healthcare providers maintain operational readiness and long-term financial performance.
Frequently Asked Questions on AI In Revenue Cycle Management
- How does AI improve claims processing?
AI supports automated claims validation, identification of coding discrepancies, and real-time error detection. As a result, claim denials are reduced, processing time is shortened, and reimbursement cycles become more efficient for hospitals and physician groups. - What benefits do healthcare providers gain from AI-enabled RCM?
Healthcare providers experience improved cash flow stability, lower administrative costs, and better compliance. Enhanced analytical capabilities support decision-making, while AI-driven automation reduces workforce strain and increases overall financial performance. - How does AI help reduce claim denials?
AI predicts denial risks by analyzing historical patterns, payer requirements, and coding accuracy. These insights allow teams to correct errors before submission, resulting in improved acceptance rates and fewer reimbursement delays. - Is AI effective in medical coding?
AI improves coding precision by interpreting clinical documentation and applying the most appropriate codes. Natural language processing strengthens accuracy and consistency, supporting compliance standards and reducing downstream billing errors. - How does AI support patient billing and collections?
AI enables personalized patient communication, transparent cost estimates, and automated reminders. These capabilities improve patient engagement, reduce payment delays, and support more predictable revenue realization for healthcare organizations. - Are there data security concerns with AI in RCM?
Data protection remains critical, and AI solutions must follow HIPAA-compliant protocols. Encryption, audit trails, and controlled access are essential to ensure safe handling of patient and financial information throughout automated RCM workflows. - Which regions are leading the AI in RCM market?
North America dominates due to advanced healthcare infrastructure, strong regulatory frameworks, and high adoption of digital technologies. Europe and Asia-Pacific are showing rapid growth as providers shift toward automation and cost-optimization strategies. - What technology trends are shaping the market?
Key trends include predictive analytics, NLP-driven coding automation, AI-based denial management, and robotic process automation. These technologies accelerate financial operations and support more accurate decision-making across the RCM ecosystem.
Conclusion
The expansion of AI in revenue cycle management has been supported by strong demand for operational efficiency, financial accuracy, and administrative automation across healthcare systems. Its adoption has enhanced claims processing, improved documentation integrity, and strengthened denial prevention measures. Service-based and integrated platforms have maintained dominant positions, while hospitals remain the primary users.
Regional growth has been led by North America, with rapid expansion projected in Asia Pacific. The market outlook remains positive as digital transformation accelerates, with AI-driven tools expected to further optimize workflows, reinforce compliance, and improve long-term financial performance for healthcare providers.
Discuss your needs with our analyst
Please share your requirements with more details so our analyst can check if they can solve your problem(s)



