Table of Contents
- Introduction
- Editor’s Choice
- Basic Flu Epidemiology Statistics
- Demographic Insights
- Flu Vaccination Statistics
- Influenza Vaccine Market Overview
- Influenza-Related Medical Visits
- Prevention Measures
- Key Funding and Investment Statistics
- Flu Treatment Statistics
- Flu Treatment Initiatives Statistics
- Flu Treatment Regulations and Statistics
- Recent Developments
- Conclusion
- FAQs
Introduction
Flu Statistics: Influenza, or the flu, is an acute respiratory illness caused by influenza viruses, primarily types A and B. It spreads through respiratory droplets and can cause symptoms such as fever, cough, sore throat, and muscle aches, with severity ranging from mild to severe.
Diagnosis is often clinical but can be confirmed through laboratory tests. Prevention is best achieved through annual flu vaccination and good hygiene practices. Antiviral medications can help if taken within 48 hours of symptom onset.
Complications include pneumonia and sinus infections, making it important for vulnerable populations to seek medical attention when needed. For updated information, it is advised to consult health organizations like the CDC or WHO.

Editor’s Choice
- The Influenza Vaccine Market size is expected to be worth around USD 6.7 billion by 2023 from USD 13.9 billion in 2033, growing at a CAGR of 7.6% during the forecast period from 2024 to 2033.
- The Spanish flu pandemic of 1918-1919 stands as the deadliest. With an estimated 50 million fatalities worldwide, making it one of the most devastating health crises in human history.
- The data on influenza and pneumonia death rates per 100,000 individuals highlight significant disparities across various countries. Lesotho exhibits the highest death rate at 192.07 per 100,000.
- During the 2022-2023 flu season in the United States. The rate of hospitalizations due to influenza varied significantly across different age groups. The highest hospitalization rate was observed among individuals aged 65 and older. With 332.4 hospitalizations per 100,000 population, highlighting the increased vulnerability of older adults to severe outcomes from influenza.
- In 2022, concerns about influenza among adults in the United States showed variations by gender. A higher proportion of women expressed concern. With 20% of females being “very concerned” about influenza, compared to 16% of males.
- The flu vaccination rates across various countries reveal significant disparities in uptake. Reflecting differing levels of public health engagement and policy effectiveness. Denmark leads with a high vaccination rate of 78%.
- With live attenuated vaccines dominating at $12.91 billion and inactivated vaccines at $0.99 billion.
- The global flu treatment market revenue is forecasted to reach $1.6 billion by 2032.
- In the 2016-2017 flu season in the United States, the costs of influenza treatments per person varied significantly depending on the type of treatment. Emergency room visits were the most expensive, with a mean cost of $840 and a median cost of $418. Highlighting the high costs associated with more acute care.
Basic Flu Epidemiology Statistics
Fatalities Due to Flu Pandemics Worldwide Statistics
- Throughout history, influenza pandemics have resulted in significant global fatalities. With varying impacts depending on the severity and reach of the virus.
- The Spanish flu pandemic of 1918-1919 stands as the deadliest. With an estimated 50 million fatalities worldwide, making it one of the most devastating health crises in human history.
- The Asian flu pandemic of 1957-1958 caused approximately 1.1 million deaths. The Hong Kong flu pandemic of 1968-1969 resulted in an estimated 1 million fatalities.
- More recently, the Swine Flu (H1N1) pandemic of 2009 led to approximately 575,400 deaths globally.
- These figures underscore the significant mortality associated with influenza pandemics and highlight the importance of preparedness and response efforts to mitigate their impact.
(Source: Statista)

Reported Cases of Influenza Worldwide by Flu Statistics
- In 2021, the worldwide reported cases of influenza were tracked weekly and categorized by type. Influenza Type A and Influenza Type B show distinct trends throughout the year.
- Early in the year, both types exhibited relatively low case numbers. With Influenza Type A starting at 149 cases and Type B at 312 cases in the first week.
- The numbers for both types remained modest through the first quarter. Fluctuating but generally staying below 300 cases per week.
- Midway through the year, a gradual increase was observed, particularly for Type A. Which saw a steady rise from around week 27. Culminating in significant spikes by week 45, where cases jumped to 1,384.
- Type B followed a similar trend, though it consistently had lower case numbers compared to Type A.
- The latter part of the year, especially from week 46 onwards, saw a dramatic escalation in cases. Week 47 reported the most significant surge, with 3,637 cases of Type A and 1,382 cases of Type B.
- The peak of reported influenza cases occurred in weeks 48 and 49. With Type A reaching its highest at 7,917 cases in week 49. While Type B also saw an increase, albeit at a slower rate, peaking at 2,283 cases in the same week.
- The year ended with a slight decline but still high numbers. With week 52 reporting 6,483 cases of Type A and 2,893 cases of Type B.
- Overall, Type A consistently had higher case numbers than Type B Especially towards the end of the year.
(Source: Statista)

Flu Statistics by Influenza and Pneumonia Deaths – By Country
- The data on influenza and pneumonia death rates per 100,000 individuals highlights significant disparities across various countries.
- Lesotho exhibits the highest death rate at 192.07 per 100,000. Followed by the Central African Republic and Somalia, with rates of 163.64 and 155.59, respectively.
- Chad and Eritrea also report notably high death rates, at 155.4 and 152.35 per 100,000.
- The Philippines stands out as the only non-African country on this list, with a death rate of 146.92 per 100,000.
- Other countries with elevated rates include Guinea (145.9), Zimbabwe (139.11), and Sierra Leone (131.43).
- Guinea-Bissau and Togo report similar figures, at 123.23 and 122.55 per 100,000, respectively, closely followed by Burkina Faso at 122.3.
- Swaziland, Niger, and Côte d’Ivoire also exhibit significant death rates. Ranging from 120.84 to 118.39 per 100,000.
- Lastly, the Democratic Republic of Congo (117.32), Cameroon (116.04), Gambia (113.77), and Mozambique (113.1) round out the list. All showing concerning levels of mortality related to influenza and pneumonia.
- These statistics underscore the severe public health challenges faced by these nations, particularly in regions of Africa.
(Source: World Life Expectancy)

Demographic Insights
Statistics By Age
Flu Statistics by Influenza-Related Hospitalizations – By Age Group
- During the 2022-2023 flu season in the United States. The rate of hospitalizations due to influenza varied significantly across different age groups.
- The highest hospitalization rate was observed among individuals aged 65 and older, with 332.4 hospitalizations per 100,000 population. Highlighting the increased vulnerability of older adults to severe outcomes from influenza.
- Children aged 0-4 years also had a notably high hospitalization rate, recorded at 125.7 per 100,000.
- The 50-64 age group experienced a hospitalization rate of 105.9 per 100,000. Indicating substantial risk in this demographic as well.
- In contrast, younger populations had lower hospitalization rates. With those aged 5-17 years and 18-49 years reporting rates of 45.9 and 44.7 per 100,000, respectively.
- These figures emphasize the differential impact of influenza across age groups. With the youngest and oldest populations being the most affected during this flu season.
(Source: Statista)

Flu Statistics by Mortality Rate for Influenza – By Age Group
- The influenza mortality rate during the 2022-2023 flu season in the United States exhibited a clear age-related pattern. With older adults facing significantly higher mortality risks.
- Individuals aged 65 and older had the highest mortality rate, at 26.6 per 100,000 population. Underscoring the severe impact of influenza on this age group.
- The mortality rate for those aged 50-64 years was 7.2 per 100,000, indicating a moderate risk for middle-aged adults. In contrast, younger age groups experienced much lower mortality rates.
- The 18-49 years age group had a rate of 0.7 per 100,000. While children aged 5-17 years had a slightly lower rate of 0.5 per 100,000.
- The youngest age group, 0-4 years, had a mortality rate of 1.2 per 100,000.
- These statistics highlight the heightened vulnerability of older populations to influenza-related fatalities compared to younger age groups during this flu season.
(Source: Statista)

By Gender
Flu Statistics by Concern About Influenza – By Gender
- In 2022, concerns about influenza among adults in the United States showed variations by gender.
- A higher proportion of women expressed concern. With 20% of females being “very concerned” about influenza, compared to 16% of males.
- Similarly, 34% of women were “somewhat concerned,” slightly more than the 32% of men who shared this sentiment.
- When it came to lower levels of concern, 25% of males reported being “not very concerned,” slightly higher than the 24% of females.
- A notable gender difference was observed among those “not at all concerned,” with 24% of men and only 17% of women falling into this category.
- Additionally, a small proportion of adults had no opinion or were uncertain. With 4% of men and 5% of women indicating that they “don’t know” or had “no opinion” on the matter.
- These figures illustrate gender-based differences in the perception of influenza risk among the U.S. adult population in 2022.
(Source: Statista)

Death Rate from Influenza and Pneumonia – By Gender
- The death rate from influenza and pneumonia in Canada from 2000 to 2022 exhibited notable fluctuations by gender.
- In the early 2000s, women consistently had higher mortality rates compared to men. Starting at 17.6 per 100,000 for females and 14.7 for males in 2000.
- This trend continued, with females maintaining higher rates throughout most of the period.
- For instance, in 2005, the female mortality rate peaked at 20.4 per 100,000. While the male rate was 15.8 per 100,000.
- A significant increase was observed in 2018 when the female death rate reached its highest at 24.7 per 100,000. While the male rate rose to 21.7 per 100,000, reflecting the severity of influenza and pneumonia during that year.
- In contrast, the lowest death rates were recorded in 2021, with females at 10.3 per 100,000 and males at 11.3 per 100,000. Likely influenced by public health measures during the COVID-19 pandemic.
- By 2022, the rates had rebounded slightly, with females at 15.2 per 100,000 and males at 15.6 per 100,000, showing a convergence in mortality rates between genders.
- Over the two decades, women generally had higher mortality rates from these illnesses. The gap between genders narrowed significantly in recent years.
(Source: Statista)

By Generation
Level of Concern About Influenza – By Generation
- In 2022, concerns about influenza among adults in the United States varied across different generations.
- Baby Boomers exhibited the highest levels of concern, with 20% reporting that they were “very concerned” and 37% indicating they were “somewhat concerned.”
- Generation X also showed significant concern, with 19% being “very concerned” and 31% “somewhat concerned.”
- Millennials followed closely, with 17% “very concerned” and 32% “somewhat concerned.” Generation Z had the lowest level of concern, with 18% “very concerned” and 27% “somewhat concerned.”
- Regarding lower levels of concern, 26% of Boomers were “not very concerned,” compared to 24% of Generation X, 22% of Millennials, and 22% of Generation Z.
- The proportion of individuals who were “not at all concerned” was highest among Generation Z and Millennials, both at 23%. While 22% of Generation X and 16% of Boomers shared this view.
- Additionally, uncertainty or lack of opinion was most common among Generation Z. With 10% indicating they “don’t know” or had “no opinion,” compared to 6% of Millennials, 4% of Generation X, and just 2% of Boomers.
- These findings reveal generational differences in the perception of influenza risk. Older generations generally express higher levels of concern compared to younger ones.
(Source: Statista)

Flu Vaccination Statistics
Flu Vaccination – According to Country Statistics
- The flu vaccination rates across various countries reveal significant disparities in uptake. Reflecting differing levels of public health engagement and policy effectiveness.
- Denmark leads with a high vaccination rate of 78%, followed closely by Ireland at 75.4% and Chile at 73.2%.
- Other countries with relatively high vaccination rates include Mexico (72.6%), the United Kingdom (72.4%), Spain (69%), and New Zealand (69%).
- The Netherlands (67.9%), the United States (67.5%), and Japan (66%) also report substantial vaccination rates.
- In contrast, several countries show moderate uptake, such as Norway (65.5%), Italy and Greece (both at 65.3%), and Canada (64.7%).
- Finland (62.7%), Australia (61.9%), Israel (61%), Costa Rica (60.6%), Sweden (60.4%), and Iceland (60.4%) hover around the 60% mark.
- France (59.9%), Belgium (59.1%), and Germany (47.3%) demonstrate lower vaccination rates. With Luxembourg (46.3%) slightly behind.
- Eastern European countries exhibit particularly low vaccination rates. With Slovenia at 27%, Lithuania at 26.3%, the Czech Republic at 23.9%, Hungary at 22.3%, Austria at 18.3%, Slovakia at 12.8%, and Estonia at 12%.
- Poland (10.4%) and Latvia (9.1%) show minimal engagement, and Turkey records the lowest rate at 5.9%.
- These figures highlight the significant variation in flu vaccination rates globally. Some countries achieve high coverage while others lag considerably behind.
(Source: World Population Review)

Influenza-Related Illnesses Prevention by Vaccination – By Age
- During the 2022-2023 flu season in the United States, influenza vaccination was estimated to prevent a significant number of influenza A- and B-associated illnesses across various age groups.
- The highest number of illnesses prevented was among children aged 5-17 years, with an estimated 1,912,522 cases avoided due to vaccination.
- In the six months to 4 years age group, vaccination prevented approximately 929,408 illnesses.
- Among adults aged 18-49 years, 1,488,913 illnesses were prevented. While in the 50-64 years age group, vaccination helped avoid 1,314,988 cases.
- The smallest number of illnesses prevented was in the 65-year-old and older age group, with an estimated 340,168 cases avoided.
- These figures highlight the substantial impact of influenza vaccination in reducing the burden of illness across all age groups, particularly among younger populations.
(Source: Statista)

Immunization of Elderly People Against Influenza
- The share of the population aged 65 or older who were immunized against influenza in Chile from 2011 to 2023 demonstrates notable fluctuations over the years.
- Immunization rates began at 62.4% in 2011, steadily increasing to a peak of 76.5% in 2013.
- However, this upward trend was interrupted in 2015 and 2016. When the immunization rates dropped significantly to 55% and 54%, respectively.
- The following years saw a gradual recovery, with the rate reaching 68.3% in 2019.
- A significant increase occurred in 2020, likely influenced by the COVID-19 pandemic. The immunization rate surged to 84.7%, the highest in the observed period.
- However, this peak was not sustained, as the rate declined to 73.2% in 2021 and continued to decrease to 70.2% in 2022 and 65.2% in 2023.
- Overall, while there has been variability in the immunization rates. The data reflects a general trend of fluctuating but relatively high levels of vaccination coverage among the elderly population in Chile over the past decade.
(Source: Statista)

Flu Vaccination Coverage Among Children – By Race/ Ethnicity Statistics
- During the 2022-23 flu season in the United States, the percentage of children aged six months to 17 years who received an influenza vaccination varied significantly by race and ethnicity.
- Overall, 57.4% of children in this age group were vaccinated against influenza.
- Among racial and ethnic groups, Asian children had the highest vaccination rate at 72.4%.
- Hispanic children also had a relatively high vaccination rate at 60.9%, above the overall average.
- White-only, non-Hispanic children had a vaccination rate of 55.6%. While Black-only, non-Hispanic children had a slightly lower rate of 53%.
- The vaccination rate among American Indian/Alaska Native (AI/AN) children was 50.6%, the lowest among the groups reported.
- Children identified as belonging to other or multiple races had a vaccination rate of 56.4%.
- These figures indicate disparities in influenza vaccination coverage among different racial and ethnic groups. Asian and Hispanic children have higher rates of vaccination compared to their peers.
(Source: Statista)

Vaccination of Flu Among College Students Statistics
- As of fall 2023, nearly half of U.S. college students reported receiving a flu vaccine within the last 12 months, with 47.4% indicating that they had been vaccinated.
- Meanwhile, 45.6% of students stated that they had not received a flu vaccine during this period.
- Additionally, 7% of students were uncertain about their vaccination status. Indicating they did not know whether they had been vaccinated against the flu in the past year.
- These statistics reflect a near-even split among college students regarding flu vaccination, with a slight majority having received the vaccine.
(Source: Statista)

Flu Vaccination Among Medicare Members Statistics
- In 2017, the percentage of Medicare enrollees who received a flu shot varied based on their type of Medicare coverage and whether they resided in urban or rural areas.
- Among Medicare Advantage members, 72.6% of those living in urban areas received a flu shot, compared to 67.8% of those in rural areas.
- Similarly, for those enrolled in the traditional fee-for-service Medicare, 71.6% of urban residents were vaccinated, while the rate was slightly lower at 67.6% for rural residents.
- These figures indicate that Medicare enrollees in urban areas had higher flu vaccination rates than their rural counterparts, regardless of the type of Medicare plan.
(Source: Statista)

Reduction of Influenza from Flu Vaccination Statistics
- From 2010 to 2016, flu vaccinations in the United States played a significant role in reducing the burden of influenza-related illnesses, medical visits, and hospitalizations, though the impact varied year by year.
- During the 2010-2011 flu season, vaccinations reduced illnesses by 19%, medical visits by 20%, and hospitalizations by 20%.
- The following year, 2011-2012, saw a similar reduction in illnesses and medical visits at 18%, while hospitalizations were reduced by 22%.
- The 2012-2013 season experienced a lower impact. With a 14% reduction in both illnesses and medical visits and a 9% reduction in hospitalizations.
- In the 2013-2014 season, vaccinations again reduced illnesses by 19%, medical visits by 20%, and hospitalizations by 21%.
- However, the 2014-2015 season marked a significant drop in effectiveness, with only a 4% reduction in illnesses, a 5% reduction in medical visits, and a 6% reduction in hospitalizations, reflecting a particularly challenging flu season.
- The 2015-2016 season showed a rebound in effectiveness, with reductions of 17% in illnesses, 18% in medical visits, and 19% in hospitalizations.
- Overall, these data illustrate the variable but generally positive impact of flu vaccinations in mitigating the effects of influenza across different seasons.
(Source: Statista)

Influenza Vaccine Market Overview
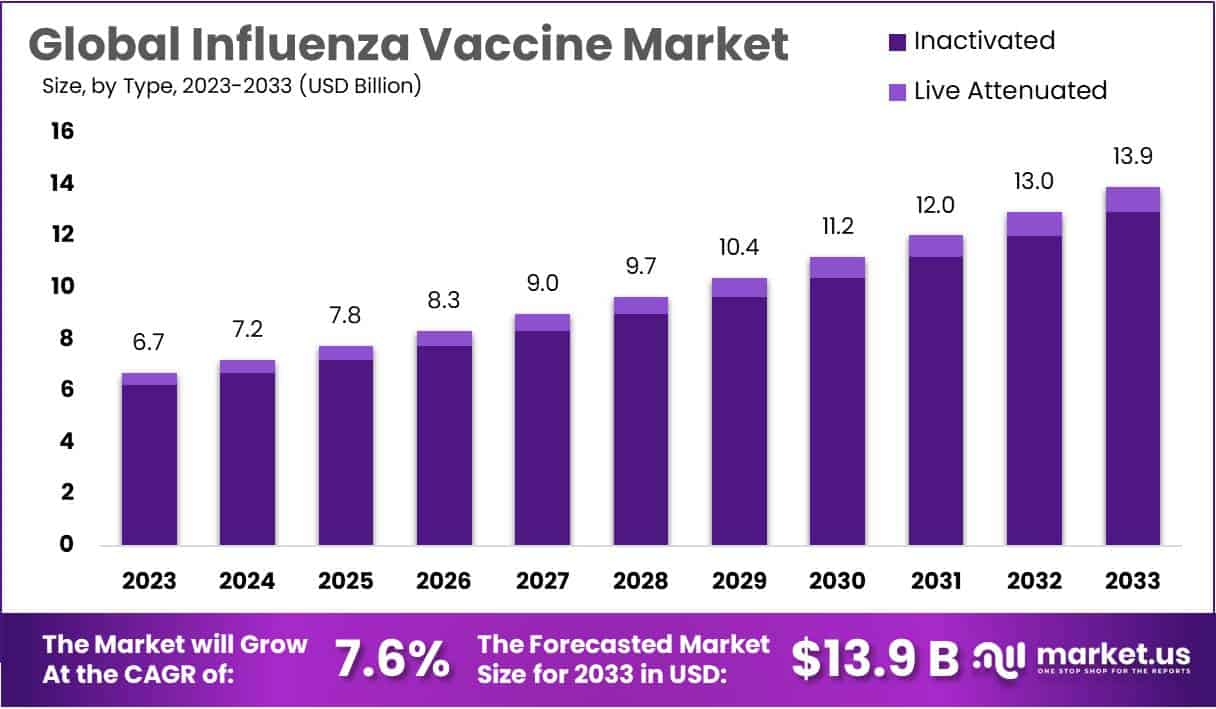
Global Influenza Vaccine Market Size
- The global influenza vaccine market is projected to experience substantial growth over the next decade at a CAGR of 7.6%.
- In 2023, the market revenue was estimated at $6.7 billion, with consistent annual increases expected after that.
- By 2024, the market is forecasted to reach $7.2 billion, and by 2025, it is anticipated to grow to $7.8 billion.
- This upward trajectory continues, with the market projected to hit $8.3 billion in 2026 and $9.0 billion in 2027.
- The growth trend accelerates further, with revenues expected to rise to $9.7 billion in 2028 and $10.4 billion in 2029.
- Entering the 2030s, the market is forecasted to expand significantly, reaching $11.2 billion by 2030 and $12.0 billion by 2031.
- By 2032, the global influenza vaccine market is expected to generate $13.0 billion in revenue, culminating in a substantial $13.9 billion by 2033.
- This consistent growth reflects increasing demand for influenza vaccines, driven by rising awareness, expanding vaccination programs, and ongoing advancements in vaccine development.
(Source: market.us)

Global Influenza Vaccine Market Size – By Type
2023-2026
- The global influenza vaccine market is expected to witness robust growth from 2023 to 2026, with both live attenuated and inactivated vaccines contributing to this expansion.
- In 2023, the total market revenue was estimated at $6.7 billion, with live attenuated vaccines accounting for $6.22 billion and inactivated vaccines contributing $0.48 billion.
- The market is projected to grow steadily, reaching $7.2 billion in 2024, with live attenuated vaccines generating $6.69 billion and inactivated vaccines $0.51 billion.
- By 2025, the market is expected to increase to $7.8 billion, with live attenuated vaccines comprising $7.25 billion and inactivated vaccines $0.55 billion.
2027-2032
- This growth trend continues annually, with the market anticipated to reach $9.0 billion in 2027, with live attenuated vaccines at $8.36 billion and inactivated vaccines at $0.64 billion.
- The market is forecasted to expand further, hitting $11.2 billion by 2030, with live attenuated vaccines contributing $10.40 billion and inactivated vaccines $0.80 billion.
- By 2033, the total influenza vaccine market is projected to reach $13.9 billion, with live attenuated vaccines dominating at $12.91 billion and inactivated vaccines at $0.99 billion.
- These figures underscore the significant role of live attenuated vaccines in driving market growth, although inactivated vaccines continue to maintain a consistent share within the expanding market.
(Source: market.us)

Global Influenza Vaccine Market Share – Age Group
- In the global influenza vaccine market, the adult age group holds a dominant position, accounting for 78.4% of the market share.
- In contrast, the pediatric segment represents 21.6% of the market.
- This distribution indicates a significantly higher demand for influenza vaccines among adults compared to children, reflecting the broader focus on vaccinating the adult population, which includes higher-risk groups such as the elderly and individuals with chronic health conditions.
- The substantial market share of the adult segment underscores the critical role of adult vaccination programs in the overall influenza prevention strategy.
(Source: market.us)

Global Influenza Vaccine Market Share – By Route of Administration
- In the global influenza vaccine market, the injection route of administration is the most prevalent, commanding 60.7% of the market share.
- This indicates that the majority of influenza vaccines are administered through injections, which are widely used due to their effectiveness and established delivery methods.
- On the other hand, nasal spray vaccines account for 39.3% of the market share, offering an alternative, needle-free option that is particularly appealing to certain populations, such as children and those with needle aversion.
- While injections dominate the market, the significant share of nasal spray vaccines reflects growing acceptance and utilization of this less invasive delivery method.
(Source: market.us)

Influenza-Related Medical Visits
- The estimated number of influenza-related medical visits in the United States has fluctuated significantly from 2010 to 2023, reflecting varying levels of influenza activity across different flu seasons.
- In the 2010-2011 season, there were approximately 10 million medical visits related to influenza.
- This number dropped sharply to 4.3 million in the 2011-2012 season, one of the lowest during this period.
- However, the 2012-2013 season saw a substantial increase, with 15 million medical visits.
- The following years continued to exhibit variability, with 13 million visits in both the 2013-2014 and 2016-2017 seasons and a peak of 18 million visits during the severe 2017-2018 flu season.
- The 2014-2015 and 2019-2020 seasons also recorded high numbers, with 14 million and 16 million visits, respectively.
- The number of medical visits dropped significantly again in the 2021-2022 season to 4.3 million, reflecting reduced flu activity, likely influenced by public health measures during the COVID-19 pandemic.
- However, by the 2022-2023 season, the number of influenza-related medical visits rebounded to 14 million.
- This data highlights the annual variability in influenza impact, influenced by the severity of the circulating strains and public health responses.
(Source: Statista)

Prevention Measures
- As of 2017, a significant portion of U.S. adults reported not taking standard precautionary measures to prevent the spread of germs the last time they had the flu or flu-like symptoms.
- Specifically, 57% of respondents indicated that they did not use disinfectant wipes on surfaces they touched, and 51% did not use hand sanitizer after coughing or sneezing.
- Additionally, 26% admitted to not washing their hands after coughing or sneezing.
- These statistics highlight gaps in adherence to recommended hygiene practices that are critical in reducing the transmission of influenza and other respiratory illnesses.
(Source: Statista)

Key Funding and Investment Statistics
- The funding allocated by the National Institutes of Health (NIH) for pneumonia and influenza research has fluctuated over the years, reflecting changes in public health priorities and funding availability.
- From FY 2013 to FY 2025, funding has generally trended upward, starting at $407 million in 2013.
- There was a slight decrease to $362 million in 2014, followed by a gradual increase in subsequent years, with $384 million in 2015 and $380 million in 2016.
- Funding reached $408 million in 2017, marking a return to the initial 2013 levels.
- A more significant increase occurred in 2018, with funding rising to $467 million and further to $521 million in 2019.
- The most substantial spike was in 2020, with funding reaching $660 million, likely in response to the heightened focus on respiratory illnesses due to the COVID-19 pandemic.
- Although there was a slight decrease to $592 million in 2021 and $578 million in 2022, funding levels rebounded in 2023 to $654 million.
- The funding is projected to stabilize, with $644 million allocated for 2024 and $646 million for 2025.
- This trajectory underscores the increasing emphasis on research and development in combating pneumonia and influenza over this period.
(Source: Statista)

Flu Treatment Statistics
Global Flu Treatment Market Revenue Statistics
- The global flu treatment market is projected to experience steady growth over the next decade at a CAGR of 4.8%, with revenues gradually increasing from $1.0 billion in 2022 to $1.6 billion by 2032.
- In 2023, the market is expected to generate $1.1 billion, maintaining this level into 2024.
- By 2025, revenues are anticipated to rise to $1.2 billion, followed by $1.3 billion in both 2026 and 2027.
- Continued growth is expected, with the market reaching $1.4 billion in 2028 and 2029.
- By 2030, the market is forecasted to reach $1.5 billion, eventually growing to $1.6 billion in both 2031 and 2032.
- This consistent upward trend reflects the ongoing demand for flu treatments and the expanding global market for such interventions.

Specific Types of Treatment for Influenza – By Age and Treatment
- During the 2016-2017 flu season in the United States, the share of people who received influenza treatment varied by age group and treatment type.
- Overall, 78.6% of individuals sought ambulatory visits, with a slightly higher rate among those under 18 years old (79.6%) compared to adults aged 18 and older (78.1%).
- The use of prescribed medicines was reported by 63.8% of individuals, with adults having a higher rate of 64.8% compared to 61.8% among those under 18.
- Emergency room visits were less common, with 11.8% of all individuals seeking this type of care. This rate was slightly lower for those under 18 years old (11.6%) and slightly higher for adults (12%).
- These figures highlight the differences in treatment-seeking behaviors across age groups, with ambulatory visits being the most common form of influenza treatment across all ages.
(Source: Statista)

Costs of Treatments for Influenza
- In the 2016-2017 flu season in the United States, the costs of influenza treatments per person varied significantly depending on the type of treatment.
- The mean cost for ambulatory visits was $312, with a median cost of $136, indicating that while some visits were relatively inexpensive, others incurred higher expenses.
- Prescribed medicines had a lower mean cost of $119 and a median cost of $43, reflecting a more affordable treatment option for many individuals.
- Emergency room visits were the most expensive, with a mean cost of $840 and a median cost of $418, highlighting the high costs associated with more acute care.
- Across all treatment categories, the overall mean cost per person was $587, with a median cost of $187, indicating that while the average cost was substantial, half of the individuals incurred costs below this level.
- These figures underscore the financial burden that influenza treatment can impose, particularly in more severe cases requiring emergency care.
(Source: Statista)

Flu Treatment Initiatives Statistics
- Recent initiatives in flu treatment are focusing on enhancing preparedness and response capabilities against both seasonal and pandemic influenza, particularly in light of emerging threats like H5N1.
- Organizations such as the World Health Organization (WHO) and the U.S. Department of Health and Human Services (HHS) have launched comprehensive strategies to bolster flu defenses globally.
- WHO’s mRNA Technology Transfer Program, in partnership with Sinergium Biotech, aims to develop and distribute advanced mRNA vaccines targeting avian influenza in low- and middle-income countries, ensuring wider access to crucial immunizations.
- Concurrently, the U.S. Administration for Strategic Preparedness and Response (ASPR) is advancing the development of novel flu vaccines and therapeutics and enhancing diagnostic tools to enable quicker and more effective treatment responses during flu outbreaks.
- These combined efforts are essential in mitigating the impact of flu on public health worldwide.
(Sources: CDC, American Hospital Association, WHO, HHS)
Flu Treatment Regulations and Statistics
- Flu treatment regulations vary widely across countries, reflecting differences in public health priorities and healthcare infrastructure.
- In the United States, the Centers for Disease Control and Prevention (CDC) provides guidelines on the use of antiviral medications and flu vaccines, emphasizing timely access to treatment for high-risk populations.
- In the European Union, the European Medicines Agency (EMA) issues annual recommendations on the composition of flu vaccines, adapting them based on evolving virus strains to ensure efficacy.
- Additionally, the World Health Organization (WHO) supports global efforts to strengthen flu vaccination programs, particularly in low- and middle-income countries, by providing technical and financial resources to ensure broader access and preparedness.
- Countries like Japan and Australia have implemented strict regulatory frameworks that mandate annual vaccinations and promote early treatment access to minimize the impact of seasonal flu.
- These regulations are part of a broader global strategy to enhance flu preparedness and response, ensuring that effective treatments and vaccines are available to populations most at risk.
(Sources: WHO, European Medicines Agency)
Recent Developments
Acquisitions and Mergers:
- Sanofi acquires Translate Bio: In early 2023, Sanofi completed its acquisition of Translate Bio, a company specializing in mRNA technology, for $3.2 billion. This acquisition aims to boost Sanofi’s flu vaccine development capabilities by leveraging mRNA technology for more effective and adaptable flu vaccines.
- CSL Limited merges with Seqirus: In mid-2023, CSL Limited, a global biotechnology company, merged its vaccine subsidiary, Seqirus, with another leading flu vaccine provider. This merger, valued at $1.5 billion, is expected to strengthen CSL’s position in the global influenza vaccine market.
New Product Launches:
- Fluad® Quadrivalent Vaccine: In 2023, Seqirus launched Fluad® Quadrivalent, an adjuvanted quadrivalent influenza vaccine designed to provide enhanced protection for older adults. This vaccine targets four different flu strains and is expected to improve immunity in the elderly population, who are at higher risk for severe flu complications.
- Moderna’s mRNA Flu Vaccine: Moderna announced the launch of a new mRNA-based flu vaccine in late 2023, aiming to offer a more effective alternative to traditional flu vaccines. This new vaccine leverages mRNA technology. Similar to the company’s COVID-19 vaccine, and is designed to be quickly adaptable to emerging flu strains.
Funding:
- NIH awards $150 million for flu research: In 2023, the National Institutes of Health (NIH) awarded $150 million in grants to various research institutions focused on developing a universal flu vaccine. The funding is part of a larger initiative to create a vaccine that offers long-term protection against multiple strains of the flu.
- GSK secures $200 million for vaccine R&D: GSK, a leading global healthcare company, secured $200 million in early 2024 to invest in the research and development of next-generation flu vaccines. With a focus on improving efficacy and reducing the need for annual vaccinations.
Technological Advancements:
- AI in Flu Prediction: The use of artificial intelligence (AI) to predict flu outbreaks has gained traction. Several healthcare organizations implementing AI-driven models to forecast flu seasons more accurately. By 2024, it is expected that over 50% of flu surveillance programs will integrate AI tools to enhance prediction accuracy and improve vaccine distribution strategies.
- Nanoparticle-Based Flu Vaccines: Researchers are developing nanoparticle-based flu vaccines that offer broader protection by targeting multiple flu strains simultaneously. These vaccines are in the advanced stages of clinical trials and could represent a significant advancement in flu prevention.
Market Dynamics:
- Growth in Flu Vaccine Market: The global flu vaccine market was valued at approximately $7 billion in 2023 and is projected to grow at a CAGR of 5.4% from 2023 to 2028. This growth is driven by increased awareness of the importance of vaccination. Government vaccination programs, and the development of more effective vaccines.
- Rising Demand for Quadrivalent Vaccines: There is a significant shift towards quadrivalent flu vaccines, which protect against four different flu strains. In 2023, quadrivalent vaccines accounted for nearly 70% of all flu vaccines administered, reflecting the growing preference for broader protection.
Conclusion
Flu Statistics – Influenza remains a significant public health challenge with widespread impacts on individuals, healthcare systems, and economies.
The need for effective prevention and treatment strategies is evident, given the varying vaccination rates, treatment costs, and mortality rates.
Vaccination is crucial in reducing flu-related illnesses, hospitalizations, and deaths. However, disparities in coverage across different demographics and regions call for targeted public health efforts.
The economic burden of influenza underscores the importance of continued investment in research, vaccine development, and preparedness.
A sustained focus on vaccination and effective treatment is essential to mitigate the virus’s seasonal and pandemic effects.
FAQs
The flu, or influenza, is a contagious respiratory illness caused by influenza viruses. It can cause mild to severe illness and, in some cases, can lead to hospitalization or death.
The flu primarily spreads through droplets made when an infected person coughs, sneezes, or talks. It can also spread by touching surfaces or objects contaminated with the virus and then touching the face.
Common symptoms include fever, cough, sore throat, runny or stuffy nose, body aches, headaches, chills, and fatigue. Some people may also experience vomiting and diarrhea, though this is more common in children.
The best way to prevent the flu is by getting an annual flu vaccine. Other preventive measures include frequent hand washing. Avoiding close contact with sick individuals, and covering your mouth and nose when coughing or sneezing.
High-risk groups include young children, elderly adults, pregnant women, and individuals with chronic health conditions such as asthma, diabetes, or heart disease.
Discuss your needs with our analyst
Please share your requirements with more details so our analyst can check if they can solve your problem(s)



