Table of Contents
Introduction
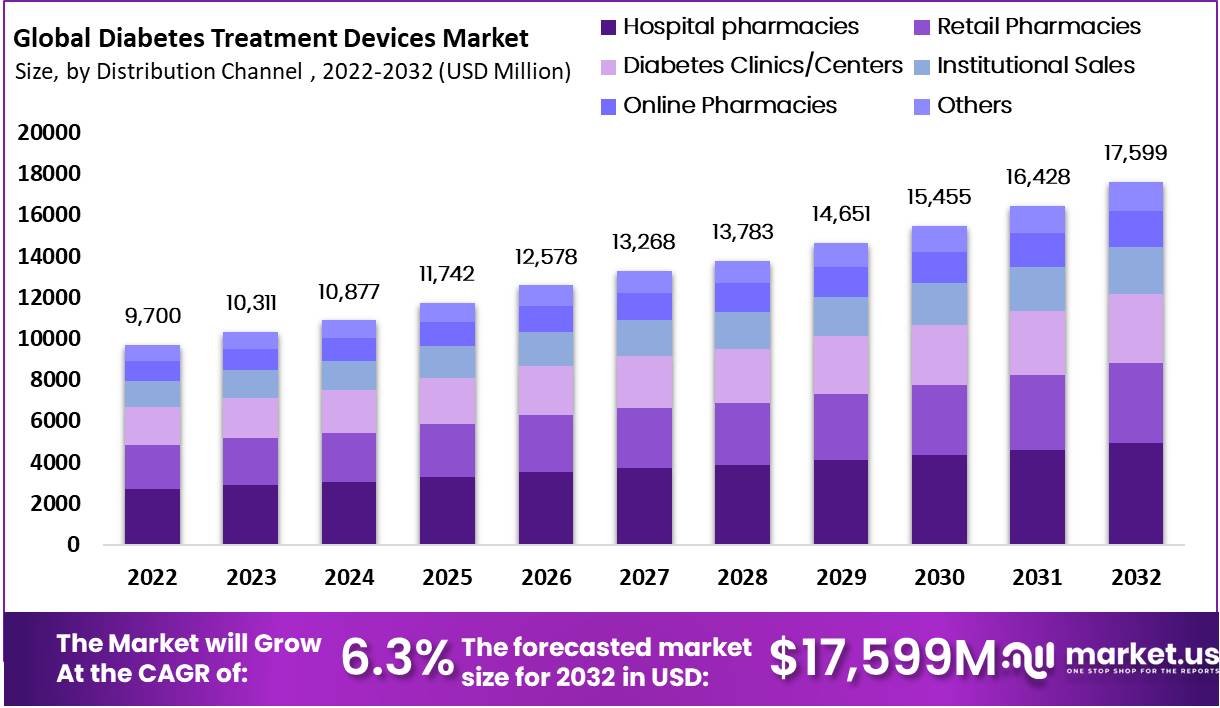
Global Diabetes Treatment Devices Market size is expected to be worth around USD 17,599 Million by 2032 from USD 9,700 Million in 2023, growing at a CAGR of 6.3% during the forecast period from 2024 to 2032.
Diabetes treatment devices are crucial tools that help manage blood glucose levels and administer insulin more efficiently, enhancing the quality of life for individuals with diabetes. Devices such as blood glucose meters and continuous glucose monitors (CGMs) provide real-time updates on blood sugar levels, significantly reducing the need for frequent finger pricks. CGMs, for example, monitor glucose levels continuously through a sensor placed under the skin, sending updates to a smartphone or other devices, alerting users to high or low levels
Insulin pumps are another vital device, offering a more automated way to deliver insulin, mimicking the body’s normal insulin release. These pumps can be programmed to dispense specific amounts of insulin automatically based on the user’s blood glucose level and can be adjusted to handle different rates of insulin delivery for varying times of the day.
Smart insulin pens have also emerged as a helpful tool, providing electronic tracking of insulin doses and integrating with digital platforms to help manage diabetes treatment effectively. These pens can record the time and amount of each dose, interfacing with mobile apps to track and analyze glucose control over time.
The global incidence of diabetes in 2019 was approximately 9.3% of the population, accounting for 463 million individuals. This number is anticipated to rise to 10.2% (578 million people) by 2030 and 10.9% (700 million people) by 2045. Urban areas exhibit a higher prevalence of diabetes at 10.8%, compared to rural areas at 7.2%. Moreover, the incidence is more prevalent in high-income countries at 10.4% versus 4.0% in low-income countries.
Remarkably, half of the individuals with diabetes (50.1%) are unaware of their condition. Additionally, the global prevalence of impaired glucose tolerance was estimated at 7.5% (374 million people) in 2019, with projections indicating an increase to 8.0% (454 million people) by 2030 and 8.6% (548 million people) by 2045.
Key Takeaways
- Market Size: Diabetes Treatment Devices Market expected to reach USD 17,599 million by 2032, growing at a 6.3% CAGR from 2022, due to rising diabetes cases.
- Market Share: The market growing at a 6.3% CAGR from 2022, due to rising diabetes cases.
- Device Types: Segmented into BGM, Continuous Glucose Monitoring, and Insulin Delivery Devices, offering diverse options.
- Distribution Channels: Include hospital pharmacies, retail pharmacies, online pharmacies, and more, adapting to consumer preferences.
- End-User Dominance: Hospitals held 40.9% of the market in 2021, while homecare is set to grow at a 7.4% CAGR.
- Drivers: Obesity rates contribute to market growth, along with government initiatives, technological innovations, and awareness campaigns.
- Regional Insights: North America dominates, benefiting from established healthcare infrastructure. The Asia-Pacific region is the fastest-growing due to increasing cancer cases.
Diabetes Treatment Devices Statistics
- Diagnosed Diabetes Prevalence in the U.S. (2021): An estimated 29.7 million individuals of all ages, or 8.9% of the U.S. population, had diagnosed diabetes.
- Diabetes Among Youth: Approximately 352,000 children and adolescents younger than age 20 had diagnosed diabetes, including 304,000 cases of type 1 diabetes.
- Insulin Use in Adults: Around 1.7 million adults aged 20 years or older, representing 5.7% of all U.S. adults with diagnosed diabetes, reported both having type 1 diabetes and using insulin.
- Early Insulin Adoption: About 3.6 million adults aged 20 years or older started using insulin within a year of their diagnosis.
- Prevalence by Ethnicity (2021):
- American Indian and Alaska Native adults: 13.6%
- Non-Hispanic Black adults: 12.1%
- Hispanic adults: 11.7%
- Non-Hispanic Asian adults: 9.1%
- Non-Hispanic White adults: 6.9%
- Cost-Effectiveness of Diabetes Management:
- Chronic Kidney Disease Screening: Annual screening costs $21,000 per quality-adjusted life year (QALY).
- Blood Pressure Management: Reduces the risk of heart disease and stroke by 33% to 50%.
- Cholesterol Improvement: Reduces cardiovascular complications by 20% to 50%.
- Eye Exams: Regular screenings could prevent up to 90% of diabetes-related blindness.
- Foot Exams: Health care services including regular foot exams could prevent up to 85% of diabetes-related amputations.
- Kidney Disease Treatment: Early treatment reduces the decline in kidney function by 33% to 37%.
- Lifestyle Modifications for Diabetes Prevention: Intensive lifestyle changes cost $12,500 per QALY, showing good value for preventing type 2 diabetes among high-risk individuals.
- Self-Monitoring of Blood Glucose: Costs $3,700 per QALY for thrice-daily monitoring compared to once daily.
- Education Level and Diabetes Prevalence:
- Adults with less than a high school education had the highest prevalence at 13.1%.
- Those with family incomes above 500% of the federal poverty level had the lowest prevalence, with 6.3% for men and 3.9% for women.
Diabetes Treatment Devices Type Analysis
- Blood Glucose Monitoring (BGM) Devices: BGM devices are essential for daily monitoring of glucose levels in individuals with diabetes. These devices require a small blood sample, usually obtained from a finger prick, and provide immediate feedback on current glucose levels. This allows for immediate management decisions regarding diet, exercise, and medication.
- Self-Monitoring Blood Glucose Devices: These devices include traditional blood glucose meters and testing strips that are used multiple times throughout the day to monitor blood glucose levels. They play a crucial role in self-management for both Type 1 and Type 2 diabetes, helping to adjust dietary intake and insulin doses based on readings.
- Continuous Glucose Monitoring (CGM) Devices: CGM devices continuously track glucose levels throughout the day and night, displaying trends that help predict increases or decreases in glucose. These devices involve a sensor inserted under the skin that sends information to a transmitter, which then relays data to a display device or a smartphone. CGMs can reduce the frequency of traditional fingerstick testing and provide detailed insights into glucose patterns.
- Insulin Delivery Devices: Insulin delivery devices range from traditional syringes to advanced insulin pumps. Syringes remain a common method for insulin delivery, requiring manual injections multiple times a day. Insulin pumps offer a more advanced alternative, delivering continuous subcutaneous insulin infusion through a catheter, providing a basal rate of insulin and allowing for bolus doses at meals. Pumps improve glycemic control and lifestyle flexibility.
- Testing Strips and Sensors: Testing strips are used with blood glucose meters to measure glucose levels at discrete points in time. Sensors, used in CGM systems, monitor glucose levels continuously and are crucial for dynamic glucose management, especially in insulin-dependent diabetes. They provide data that can inform the adjustment of therapy in real-time, crucial for avoiding both hyperglycemia and hypoglycemia.
- Transmitters: In CGM systems, transmitters play a critical role by sending data from the glucose sensor to a receiver or a connected device such as a smartphone or tablet. This allows for real-time glucose monitoring and alerts, which are essential for making immediate adjustments to therapy.
Emerging Trends
- Integration of Digital Tools in Diabetes Management: Recent trends show a significant move towards integrating digital tools into diabetes management. These include smart insulin pens that can track dosage and timing, and apps that monitor blood glucose levels in real-time. These tools aim to enhance patient adherence and improve glycemic control by providing more personalized and accessible care options.
- Global Diabetes Compact Initiative: The WHO launched the Global Diabetes Compact, aiming to ensure global access to diabetes care. This initiative focuses on improving the availability and affordability of diabetes care worldwide, especially insulin and blood glucose monitors. It seeks to set global targets to enhance the diagnosis and treatment of diabetes, aiming for widespread impact by 2030.
- Development of Closed-loop Systems: The advancement of closed-loop systems or “artificial pancreas” devices represents a significant innovation. These systems automate blood sugar management by combining insulin pumps and continuous glucose monitors with algorithms to adjust insulin delivery in real time based on glucose readings, thus helping to reduce the burden of daily diabetes management.
- Adoption of Telemedicine in Diabetes Care: Telemedicine has become more prevalent in managing diabetes, particularly highlighted during the COVID-19 pandemic. It includes virtual consultations and remote monitoring, allowing for continuous care without the need for physical clinic visits. This trend is especially beneficial in rural or underserved areas where access to endocrinologists is limited.
- Global Coverage Targets for Diabetes: The WHO has established global coverage targets to combat diabetes effectively. By 2030, these targets aim for 80% of people with diabetes to be diagnosed and have good control of their blood glucose and blood pressure, among other metrics. This strategy is part of a broader effort to integrate diabetes treatment into national noncommunicable disease programs, enhancing overall health outcomes.
Use Cases
- Remote Patient Monitoring for Chronic Diabetes Management: Diabetes treatment devices that enable remote monitoring have become crucial for managing chronic diabetes effectively. Devices like continuous glucose monitors (CGMs) and smart insulin pumps can transmit real-time data to healthcare providers. This technology supports proactive adjustments in therapy, potentially reducing emergency visits and hospitalizations by catching anomalies early. Such systems are particularly valuable in managing Type 1 diabetes and severe Type 2 diabetes.
- Integration with Telehealth Services: During the COVID-19 pandemic, telehealth has surged as a vital service for diabetes management. Diabetes devices that integrate with telehealth platforms allow patients to receive comprehensive care remotely. For example, data from CGMs and insulin pumps can be reviewed during a virtual consultation, enabling personalized treatment adjustments without needing an in-person visit.
- Preventive Care and Lifestyle Management: Wearable diabetes devices that track and analyze multiple health metrics can encourage better lifestyle management. By monitoring blood glucose levels, physical activity, and diet, these devices provide feedback that can help prevent the progression of diabetes or manage existing conditions more effectively. This is particularly useful in Type 2 diabetes, where lifestyle plays a significant role.
- Enhanced Pediatric Diabetes Care: For children with diabetes, especially Type 1, wearable devices that continuously monitor glucose levels can alert parents and caregivers to potential dangers such as hypoglycemia during the night. This use case significantly reduces anxiety and improves quality of life for both patients and their families by ensuring safety through round-the-clock monitoring.
- Data-driven Personalized Medicine: Advanced analytics capabilities of modern diabetes devices can predict patient-specific trends and potential future complications. This allows healthcare providers to customize treatment plans based on predictive insights rather than just reactive data, leading to more effective management of the disease with potentially fewer complications.
Conclusion
The proliferation of diabetes treatment devices, including blood glucose monitors, continuous glucose monitoring systems, insulin delivery devices, and smart insulin pens, has revolutionized diabetes management, enabling more precise and real-time tracking of glucose levels. These innovations not only enhance individual care but also integrate with digital health tools, improving access and adherence to treatment. As global diabetes prevalence continues to rise, these devices are essential in mitigating the disease’s impact through improved management and preventive care. They hold significant promise for advancing personalized medicine and expanding telehealth services, thereby optimizing healthcare delivery and patient outcomes.


