Table of Contents
Introduction
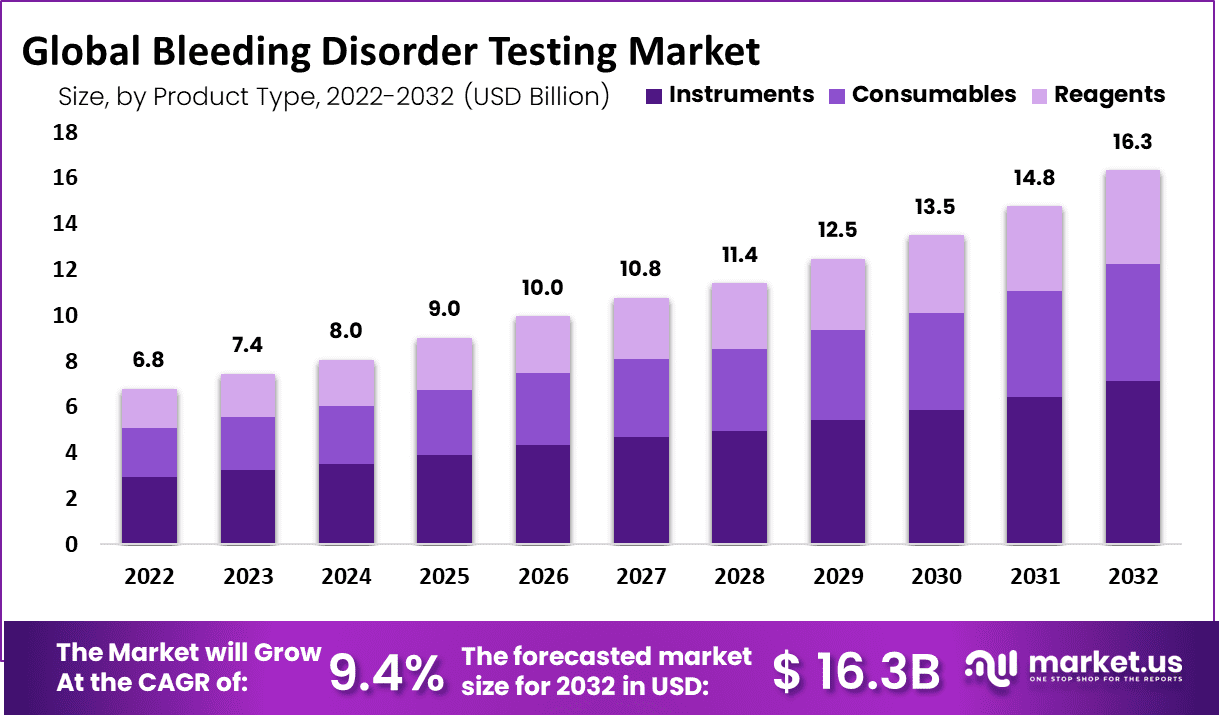
The Global Bleeding Disorder Testing Market is projected to reach USD 16.3 billion by 2032, up from USD 6.8 billion in 2022, growing at a CAGR of 9.4% from 2022 to 2032. This growth is driven by rising disease prevalence, technological advancements, government support, increased healthcare spending, and awareness campaigns. As diagnostic capabilities improve, early detection and effective treatment strategies are becoming more accessible.
The increasing prevalence of bleeding disorders is a major growth driver. Hemophilia affects approximately 1 in 5,000 male births in the U.S., with 30,000 to 33,000 affected males nationwide. Similarly, von Willebrand disease (VWD) is the most common inherited bleeding disorder, impacting around 1% of the U.S. population, or 3.2 million individuals. These numbers highlight the need for accurate diagnostic solutions to facilitate early detection and treatment. As awareness grows, healthcare providers are prioritizing routine testing for individuals at risk, further driving market expansion.
Technological innovations are revolutionizing bleeding disorder testing. Next-generation sequencing, automated coagulation analyzers, and point-of-care testing devices have improved the accuracy and efficiency of diagnostics. These advancements enable early and precise detection of both inherited and acquired bleeding disorders. Faster and more reliable tests reduce the risk of complications, leading to better patient outcomes. The introduction of AI-driven diagnostic tools and molecular testing is expected to further improve disease identification and management in the coming years.
Government initiatives and funding programs significantly contribute to market growth. The CDC’s Community Counts program collects health data from individuals with bleeding disorders, helping researchers track complications, treatment trends, and overall patient health. Increased public and private investments in diagnostic research further accelerate innovation. Additionally, growing healthcare expenditures globally have improved infrastructure and accessibility, ensuring that advanced diagnostic solutions reach a wider population. Higher diagnostic adoption rates are expected as more healthcare systems integrate modern testing technologies.
Educational initiatives and public health campaigns have increased awareness about bleeding disorders and the importance of early diagnosis. Patients and healthcare providers now recognize the need for early screening and intervention, leading to higher demand for testing services. Better awareness results in timely medical intervention, improved patient care, and reduced long-term complications. As knowledge spreads through digital platforms and healthcare programs, testing rates are expected to rise, reinforcing market growth.
The bleeding disorder testing market is expanding due to the rising prevalence of these conditions, advancements in diagnostic technology, supportive government initiatives, increased healthcare spending, and growing awareness. These factors collectively ensure early detection, improved patient outcomes, and sustained market growth.
Key Takeaways
- Market Expansion: The bleeding disorder testing market is projected to grow at a 9.4% CAGR, reaching USD 16.3 billion by 2032, driven by rising diagnosis rates.
- Key Segment Growth: Reagents and consumables are expected to see substantial growth, fueled by increased testing rates, especially in developing regions with expanding healthcare access.
- Hemophilia A Influence: Hemophilia A, affecting 1 in 10,000 people, significantly drives market demand as awareness and early diagnosis efforts improve globally.
- Diagnostic Centers Rising: Increased awareness and better diagnostic capabilities are pushing diagnostic centers to become a key segment in the bleeding disorder testing market.
- Market Growth Factors: A growing patient population, ongoing R&D, and a strong focus on recombinant DNA products are fueling market expansion and innovation.
- Challenges to Growth: Limited testing accessibility, a shortage of skilled professionals, and high treatment costs are restricting the market’s full potential, especially in emerging regions.
- Emerging Market Trends: Industry consolidation, increased R&D funding, and continuous technological advancements are shaping the future of the bleeding disorder testing market.
- North America & Europe Lead: Strong healthcare infrastructure, regulatory approvals, and early adoption of new technologies position these regions as dominant market players.
- Asia-Pacific Expansion: The Asia-Pacific market is expected to witness rapid growth, driven by improved healthcare access and rising investment in diagnostic testing.
- South America’s Potential: Ongoing genetic disease cases and growing interest in personalized medicine are positioning South America for impressive market growth in the coming years.
Emerging Trends
- Advancements in Diagnostic Technologies: Microfluidic devices are transforming bleeding disorder diagnostics. These devices replicate human-like blood flow conditions, allowing real-time observation of platelet behavior and clot formation. Traditional animal models fail to provide accurate results because they do not fully replicate human hemostasis. However, microfluidic technology offers a more precise representation. This advancement improves diagnostic accuracy and enhances treatment decisions. By mimicking real blood flow, these devices help identify clotting disorders more effectively. Researchers continue to refine this technology to increase its reliability and accessibility. The adoption of microfluidic systems in clinical settings is expected to improve early diagnosis, leading to better patient outcomes.
- Integration of AI and Nanotechnology: Artificial Intelligence (AI) and nanotechnology are improving bleeding disorder testing. AI enhances diagnostic accuracy by quickly analyzing large data sets, identifying patterns, and detecting abnormalities. Nanotechnology plays a crucial role by enabling highly sensitive blood tests. In tuberculosis testing, AI and nanotechnology have improved precision, demonstrating their potential in bleeding disorder diagnostics. By combining these innovations, researchers aim to develop faster, more reliable, and minimally invasive tests. These advancements could replace traditional lab-based methods, reducing wait times and improving accessibility. As AI-driven diagnostics evolve, healthcare providers can offer more personalized treatment plans based on highly accurate test results.
- Focus on Women’s Health: New guidelines emphasize the need for better screening of bleeding disorders in women and girls. Many cases go undiagnosed due to a lack of awareness and testing. Conditions such as von Willebrand disease (VWD) require early detection, particularly during pregnancy, surgery, and medical emergencies. Healthcare organizations now recommend routine evaluations for women with heavy menstrual bleeding or unexplained bruising. These screenings help in identifying underlying conditions that affect clotting. Early detection allows doctors to provide better treatment plans and prevent complications. Increased awareness and education among healthcare providers and patients can improve diagnosis rates and overall care.
- Enhanced Screening in Child Abuse Cases: Screening for bleeding disorders is critical in suspected child abuse cases. However, studies show that adherence to recommended testing is low. Only 9.5% of bruising cases and 32.5% of intracranial hemorrhage cases receive complete evaluations. This gap in testing can lead to misdiagnosis or wrongful accusations. Experts stress the importance of following standardized screening protocols to differentiate between medical conditions and physical abuse. Improved guidelines and increased awareness among medical professionals can enhance testing rates. More reliable screening ensures accurate assessments, reducing the risk of incorrect conclusions. Strengthening compliance with these protocols is essential for fair and accurate medical evaluations.
Use Cases
- Early Diagnosis and Management: Timely testing helps detect bleeding disorders early, enabling prompt treatment. This reduces severe bleeding episodes and improves patient outcomes. In the U.S., the median diagnosis age varies by severity. Mild hemophilia is diagnosed at 36 months, moderate at 8 months, and severe at 1 month. Early detection allows for better preventive strategies, reducing complications. It also improves the quality of life by helping patients manage symptoms effectively. Without early diagnosis, patients may experience frequent, uncontrolled bleeding, leading to joint damage or life-threatening complications. Testing also ensures healthcare providers can implement personalized care plans.
- Preoperative Assessment: Bleeding disorder testing is crucial before surgery. It identifies patients at risk of excessive bleeding. This helps surgeons plan safer procedures and choose the right interventions. Testing ensures the use of proper perioperative management strategies, such as clotting factor replacement or antifibrinolytics. These measures reduce complications and improve recovery. Without preoperative screening, patients with undiagnosed bleeding disorders face high surgical risks. Postoperative bleeding can lead to prolonged hospital stays or additional surgeries. By incorporating bleeding disorder testing in routine surgical assessments, healthcare providers can improve patient safety and surgical outcomes.
- Monitoring Anticoagulant Therapy: Patients on anticoagulants need regular bleeding disorder tests. These tests help monitor their clotting function and prevent complications. Proper management is essential, especially in trauma patients. Too much anticoagulation increases bleeding risk, while too little raises the chance of clots. Frequent testing ensures the right balance. It allows doctors to adjust dosages and prevent life-threatening complications. Without monitoring, patients may experience uncontrolled bleeding or strokes. For those on long-term therapy, routine testing is a key part of care. It provides accurate data to guide treatment and ensures a safer approach to anticoagulation management.
- Diagnosis of Unexplained Bleeding: Some patients experience abnormal bleeding with no clear cause. Standard tests may appear normal, making diagnosis challenging. Bleeding disorder testing helps identify hidden conditions like Bleeding Disorder of Unknown Cause (BDUC). Around 70% of patients referred for bleeding assessments do not receive a definitive diagnosis. Comprehensive testing can uncover rare disorders or mild clotting deficiencies. Without proper diagnosis, patients may continue experiencing unexplained symptoms. This can lead to unnecessary treatments or delays in effective care. Testing provides clarity, guiding appropriate management strategies. It also helps doctors rule out other medical conditions, improving patient outcomes.
- Screening in Suspected Child Abuse: Bleeding disorder testing plays a crucial role in child abuse investigations. It helps differentiate between medical conditions and physical abuse. Some children may have undiagnosed bleeding disorders that cause frequent bruising or unexplained bleeding. Testing ensures an accurate diagnosis, preventing wrongful accusations. Without proper screening, families may face unnecessary legal consequences. Medical professionals rely on these tests to provide evidence-based conclusions. This supports fair investigations and protects children from misdiagnosis. Healthcare providers should consider bleeding disorder screening in suspected abuse cases to ensure accurate assessments and appropriate interventions.
- Women’s Health: Many women with bleeding disorders remain undiagnosed. Conditions like von Willebrand Disease (VWD) cause heavy menstrual bleeding or postpartum hemorrhage. In Canada, an estimated 37,500 women have bleeding disorders, yet only 8,000 (20%) are diagnosed. Targeted testing helps detect these conditions early. Without testing, women may suffer from chronic anemia, fatigue, and complications during childbirth. Awareness and screening can improve treatment access. Doctors can offer personalized therapies, improving women’s quality of life. Increased testing efforts are needed to close the diagnosis gap and ensure women receive the necessary care.
- Detection of Inhibitors in Hemophilia Patients: Regular testing is essential for hemophilia patients. Some develop inhibitors that block treatment effectiveness, making standard therapies ineffective. Patients with hemophilia or von Willebrand Disease (VWD) type 3 require annual testing. Early detection of inhibitors allows for treatment adjustments, reducing complications. Without testing, patients may experience frequent bleeding episodes and reduced treatment response. Testing ensures doctors can switch to alternative therapies when needed. This proactive approach prevents severe health issues and improves patient outcomes. By making inhibitor testing a routine practice, healthcare providers can offer better, more personalized care.
Conclusion
The bleeding disorder testing market is growing due to rising disease prevalence, technological advancements, and increased awareness. Improved diagnostic tools are making early detection more accessible, leading to better treatment outcomes. Governments and healthcare organizations are investing in research and screening programs, ensuring wider access to advanced testing solutions. AI-driven diagnostics and molecular testing are transforming the industry, making testing more efficient and accurate. Increased screening for women’s health and child abuse cases highlights the expanding applications of bleeding disorder diagnostics. With strong healthcare infrastructure in key regions and rapid expansion in emerging markets, the industry is set to witness steady growth, driven by innovation, research funding, and a growing focus on preventive healthcare.
Discuss your needs with our analyst
Please share your requirements with more details so our analyst can check if they can solve your problem(s)



