Antimicrobial resistance statistics provide valuable insights into the magnitude of the problem and its impact on various aspects of health and society.
These statistics help policymakers, healthcare professionals, researchers, and the public to understand the urgency of the issue and take appropriate actions to combat it effectively.

Table of Contents
- Editor’s Choice
- What is Antimicrobial Resistance?
- Healthcare-Associated Infections and Community-Setting
- Impact of Antimicrobial Resistance Statistics
- Factors Contributing to Antimicrobial Resistance Statistics
- Strategies for Combating Antimicrobial Resistance
- Regional and Country-Specific Statistics
- Recent Developments
- Conclusion
- FAQs
Editor’s Choice
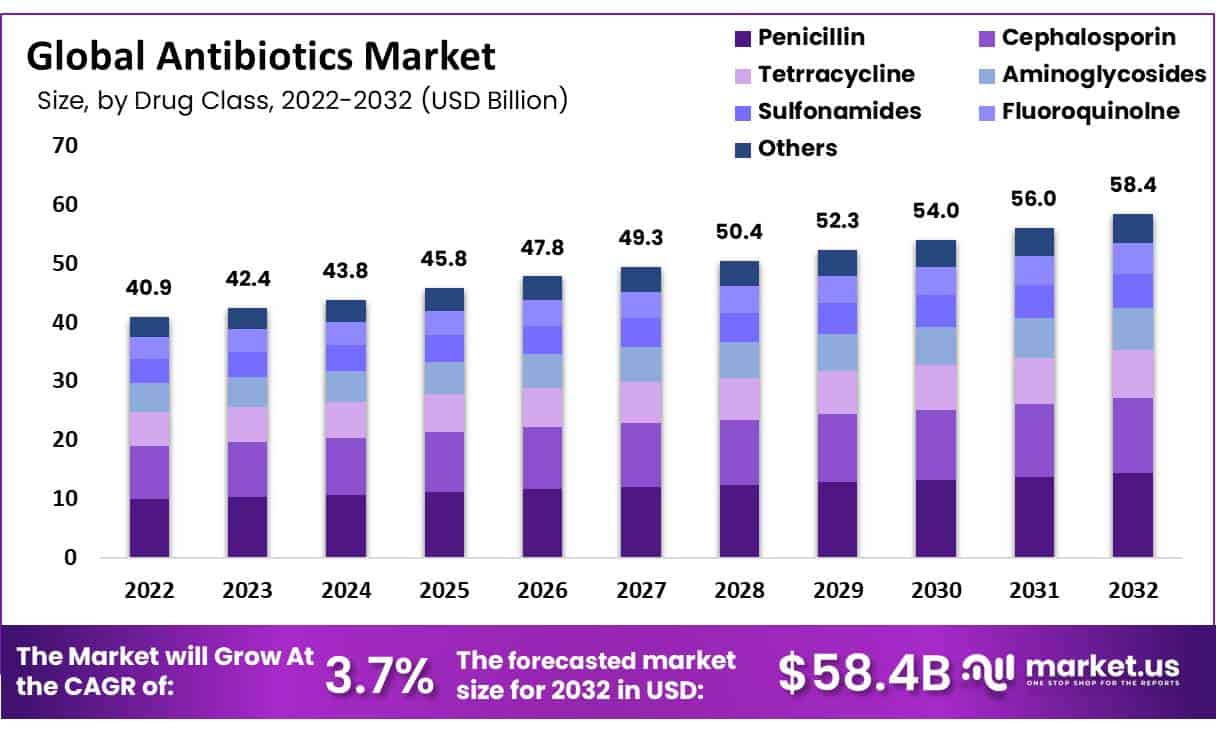
- The global Antibiotics Market size is expected to be worth around USD 58.4 Billion by 2032 from USD 40.9 Billion in 2022, growing at a CAGR of 3.7% during the forecast period from 2023 to 2032.
- By 2050, an estimated 10 million lives could be lost annually due to drug-resistant infections.
- AMR could cause global economic damage on par with the 2008 financial crisis if not addressed promptly.
- The annual cost of AMR in the United States alone is projected to reach $65 billion by 2050.
- Each year at least 700,000 deaths worldwide are attributed to antibiotic-resistant infections.
- Drug-resistant infections could cause 10 million deaths annually by 2050, surpassing deaths from cancer.
- Approximately 25,000 people in Europe die each year from infections caused by drug-resistant bacteria.
- In the United States, at least 2.8 million antibiotic-resistant infections occur annually, resulting in over 35,000 deaths.
- Carbapenem-resistant Enterobacteriaceae (CRE)infections have a mortality rate as high as 50% in some cases.
(Source: World Bank Group, Review on Antimicrobial Resistance, 2014, CDC, WHO)
What is Antimicrobial Resistance?
Antimicrobial resistance (AMR) refers to the ability of microorganisms, such as bacteria, viruses, fungi, and parasites, to develop resistance or become immune to those that are designed to kill or inhibit their growth.
It is a natural biological phenomenon that occurs when microorganisms adapt and evolve in response to the use of antimicrobial drugs.
Antimicrobial Resistance Statistics – Prevalence Worldwide
- In some countries, up to 82% of Escherichia coli infections are resistant to fluoroquinolone antibiotics, a common class of antibiotics.
- Resistance to third-generation cephalosporins, a critical class of antibiotics, has been reported in more than 50% of Klebsiella pneumonia infections in some countries.
- The prevalence of multidrug-resistant tuberculosis (MDR-TB) is estimated to be around 3.4% among previously treated cases.
- Carbapenem-resistant Enterobacteriaceae (CRE) infections have been reported in healthcare settings worldwide, with prevalence rates ranging from less than 1% to over 50% in some countries.
- Methicillin-resistant Staphylococcus aureus (MRSA) infections have been reported in both healthcare and community settings globally, with prevalence rates ranging from less than 1% to over 50% in some countries.
- Vancomycin-resistant Enterococcus (VRE) infections have been documented in various regions, with prevalence rates ranging from less than 1% to over 60% in some countries.
- Developing countries bear a disproportionately high burden of AMR due to various factors, including limited access to healthcare and inappropriate use of antibiotics.
- In low- and middle-income countries, up to 90% of Escherichia coli infections, a common cause of urinary tract and bloodstream infections, are resistant to commonly used antibiotics.
- In some developing countries, the prevalence of methicillin-resistant Staphylococcus aureus (MRSA) infections can exceed 50% in certain healthcare settings.
- In some parts of the world, such as certain regions in Asia and the Mediterranean area, CRE rates in healthcare settings can exceed 50%.
- CRE infections have high mortality rates, ranging from 40% to over 50% in some studies.
(Source: WHO)

Healthcare-Associated Infections and Community-Setting
- Approximately 7% to 10% of patients in developed countries acquire at least one healthcare-associated infection during their hospital stay.
- In the United States, it is estimated that about 1 in 31 hospital patients has at least one healthcare-associated infection at any given time.
- Methicillin-resistant Staphylococcus aureus (MRSA) is a common drug-resistant bacterium associated with healthcare settings.
- In the United States, approximately 80,461 invasive MRSA infections occur annually, resulting in around 11,285 deaths.
- In the United States, an estimated 13,100 Carbapenem-Resistant Enterobacteriaceae (CRE) infections occur annually, leading to around 1,100 deaths.
- CDI is a common healthcare-associated infection, particularly associated with antibiotic use.
- In the United States, it is estimated that there are around 223,900 cases of CDI and 12,800 deaths annually.
- In some countries, up to 90% of antibiotic use occurs in community settings, such as primary care clinics and outpatient settings.
- In the United States, about 30% of antibiotics prescribed in outpatient settings are unnecessary.
(Source: WHO, CDC)
Impact of Antimicrobial Resistance Statistics
Healthcare-associated Infections (HAIs)
- Approximately 700,000 deaths globally are attributed to HAIs caused by drug-resistant pathogens.
- In the United States, around 2 million people acquire HAIs each year, resulting in an estimated 99,000 deaths.
- In the United States, it is estimated that approximately 1 in 31 hospitalized patients have at least one HAI at any given time.
- In Europe, an estimated 4.2 million patients acquire HAIs each year, resulting in approximately 37,000 deaths directly attributed to these infections.
(Source: WHO, ECDC)
Treatment Failure Rates
- The failure rate of antibiotics commonly used to treat UTIs caused by Escherichia coli increased from 5.7% in 2011 to 13.9% in 2017.
- Approximately 60% of UTIs worldwide are caused by multi-drug-resistant bacteria.
- The treatment failure rate for community-acquired pneumonia caused by Streptococcus pneumonia ranges from 17% to 26% due to antibiotic resistance.
- Globally, an estimated 81% of countries have reported cases of gonorrhea with resistance to at least one commonly used antibiotic.
- Multi-drug-resistant tuberculosis (MDR-TB) has a treatment success rate of only 57%, significantly lower than drug-susceptible TB.
(Source: CDC, WHO)
Increased Healthcare Costs
- The global economic impact of AMR could range from $2 trillion to $100 trillion by 2050 if not effectively addressed.
- In high-income countries, the cost of AMR-related infections could amount to 2-3% of gross domestic product.
- Treating antibiotic-resistant infections in the United States adds an estimated $20 billion in direct healthcare costs annually.
- Hospitalizations due to drug-resistant infections in the U.S. cost an average of $34,000 per patient, which is 1.5 times higher than hospitalizations caused by non-resistant infections.
- AMR-related healthcare costs in the European Union are estimated to be around €1.5 billion per year.
- The annual cost of AMR-related infections in Europe, including direct healthcare costs and productivity losses, is estimated to be €7.1 billion.
- In low- and middle-income countries, the economic burden of AMR is significant. By 2050, it is estimated that AMR could push up to 28.3 million people into extreme poverty.
(Source: Review on Antimicrobial Resistance, CDC, European Commission, World Bank)
Mortality Rates – By Antimicrobial Resistance Statistics
- According to a review on antimicrobial resistance, if left unaddressed, drug-resistant infections could cause 10 million deaths annually by 2050.
- In Europe, AMR is responsible for an estimated 33,000 deaths each year.
- In the United States, it is estimated that drug-resistant infections cause over 35,000 deaths annually.
- In the United States, Methicillin-resistant Staphylococcus aureus (MRSA) infections are estimated to cause around 10,000 deaths each year.
- Globally, approximately 240,000 deaths occur annually due to MDR-TB.
(Source: CDC, WHO)

Factors Contributing to Antimicrobial Resistance Statistics
Misuse and Overuse of Antibiotics
- Global antibiotic consumption reached 34.8 billion defined daily doses (DDD), with an average consumption rate of 21.1 DDD per 1,000 inhabitants per year.
- Antibiotic consumption rates vary widely across countries, ranging from less than 10 DDD per 1,000 inhabitants per day to more than 60 DDD per 1,000 inhabitants per day.
- In high-income countries, around 20-50% of antibiotics prescribed in outpatient settings are considered unnecessary or inappropriate.
- A systematic review found that the global median prevalence of inappropriate antibiotic prescriptions in primary care was 52%, ranging from 8% to 100% across different studies and regions.
- In a study across 36 countries, the median prevalence of antibiotic purchase without a prescription was 32%, ranging from 4% to 77%.
- In low- and middle-income countries, the availability of antibiotics without a prescription can exceed 50%.
(Source: The Lancet Infectious Diseases, BMJ Global Health, PLoS ONE)
Agricultural Practices – by Antimicrobial Resistance Statistics
- Approximately 73% of global antimicrobial consumption is used in animal agriculture, primarily for growth promotion and disease prevention.
- In some countries, such as China and the United States, over 50% of antimicrobial agents produced are used in animal agriculture.
(Source: WHO)
Lack of Access to Clean Water and Sanitation
- Approximately 2.2 billion people worldwide lack access to safely managed drinking water services.
- Around 4.2 billion people globally lack access to safely managed sanitation services.
- It is estimated that approximately 800,000 deaths per year are caused by diarrheal diseases, many of which are attributed to poor water and sanitation conditions.
(Source: WHO)
Global Travel and Migration
- Studies have shown that travelers are more likely to carry drug-resistant bacteria compared to non-travelers. The prevalence of multidrug-resistant bacteria among travelers ranged from 2% to 50%, depending on the destination and risk factors.
- The risk of acquiring drug-resistant infections during international travel is estimated to be 20% to 30% higher than in non-travelers.
- A study analyzing the genetic relatedness of methicillin-resistant Staphylococcus aureus (MRSA) strains found that international travel accounted for 20% to 50% of MRSA transmission events.
- It is estimated that each year, over 200 million travelers are at risk of acquiring drug-resistant infections during international trips.
(Source: Journal of Travel Medicine, The Lancet Infectious Diseases)
Weak Healthcare Systems
- In Low- and middle-income, it is estimated that hand hygiene compliance rates among healthcare workers are generally below 50%.
- In Africa, only 28% of healthcare facilities have basic water services, and 19% lack sanitation services.
- In low-income countries, only 34% have access to a clinical microbiology laboratory, and 15% have access to antibiotics susceptibility testing.
- In sub-Saharan Africa, only 20% of countries have national surveillance systems for AMR.
- In sub-Saharan Africa, the average density of physicians is approximately 2.6 per 10,000 populations, compared to the global average of 15.1 per 10,000 populations.
(Source: WHO)

Strategies for Combating Antimicrobial Resistance
Stewardship Programs
- Implementation of stewardship programs in healthcare facilities has also been shown to reduce inappropriate antibiotic use by 20% to 50%.
- A study conducted in large hospitals in the United States reported a 47% decrease in broad-spectrum antibiotic use following the implementation of the stewardship program.
- Studies estimated that implementing stewardship programs in a large teaching hospital could save approximately $900,000 annually.
(Source: American Journal of Health-System Pharmacy)
Improved Diagnostics – Antimicrobial Resistance Statistics
- The rapid diagnostics tests could reduce unnecessary antibiotic use by 20% to 50%.
- A study conducted in a pediatric hospital in the United States demonstrated that implementing rapid diagnostic testing for bloodstream infections led to a 54% reduction in broad-spectrum antibiotic use.
(Source: JAMA)
Vaccination Programs – by Antimicrobial Resistance Statistics
- In the United States, the implementation of PCV7 (which covers 7 serotypes) is among children under 5 years old.
- PCV13 has shown a substantial reduction in antibiotic resistance to invasive pneumococcal diseases globally.
- A study in Kenya reported a 72% decline in invasive Hib disease cases following the introduction of Hib vaccination.
- A systematic review estimated that influenza vaccination reduces antibiotic prescriptions by approximately 28% during the influenza season.
(Source: The Lancet Infectious Diseases)
Regional and Country-Specific Statistics
United States
- At least 2.8 million people acquire antibiotic-resistant infections each year in the US.
- Drug-resistant infections result in more than 35,000 deaths annually in the United States.
- MRSA infections cause over 80,000 invasive infections and 11,000 deaths annually in the United States.
- Clostridioides difficile infections, often associated with antibiotic use, result in around 223,900 cases and 12,800 deaths per year in the US.
- Clostridioides difficile is responsible for more than $1 billion in excess medical costs annually.
- In 2022, there were an estimated 13,100 CRE infections in the United States, resulting in approximately 1,100 deaths.
(Source: CDC)
Europe
- In the European Union and European Economic Area, around 33,000 deaths per year are attributed to infections caused by antibiotic-resistant bacteria.
- The estimated annual healthcare cost associated with AMR in the European Union is approximately €1.5 billion.
- The burden of AMR is expected to increase, with estimates suggesting that by 2050, drug-resistant infections could cause 390,000 deaths annually in Europe if no action is taken.
- Methicillin-resistant Staphylococcus aureus (MRSA) reported ranges from 5% to 60% in healthcare settings.
- Carbapenem-resistant Enterobacteriaceae (CRE) prevalence rate exceeding more than 10%.
(Source: ECDC)
India
- It was found that 71% of clinical isolates of Klebsiella pneumonia in India were resistant to carbapenems.
- According to the World Health Organization (WHO), in 2020, an estimated 2.6 million new cases of TB occurred in India, and around 120,000 cases were classified as MDR-TB.
- A study conducted in 2021 found that nearly 77% of antibiotics in India were sold without a prescription.
(Source: Indian Journal on Medical Research)
South Africa
- A study conducted in South African hospitals found that approximately 62% of Staphylococcus aureus bloodstream isolates were methicillin-resistant.
- Approximately 3.4% of new tuberculosis cases in South Africa are estimated to be multidrug-resistant tuberculosis (MDR-TB), and 18.7% of previously treated cases are estimated to be MDR-TB.
- In 2019, sub-Saharan Africa had the highest mortality rate attributable to AMR, with 23.5 deaths per 100,000 population.
(Source: NIH)
United Kingdom
- In the UK, it is estimated that around 5,000 deaths each year are attributed to drug-resistant infections.
- In 2022, there were 1,606 MRSA bloodstream infections reported, representing a 95% reduction since 2003.
- Between 2013 and 2019, there was a 17% reduction in the number of antibiotic prescriptions issued by general practitioners.
(Source: UK Government)
Recent Developments
Research and Development Initiatives:
- Pharmaceutical companies invested in the development of new antibiotics and alternative treatments for drug-resistant infections, with a focus on novel mechanisms of action and combination therapies.
- Research institutions collaborated on studies to better understand the mechanisms of antimicrobial resistance, identify emerging resistance patterns, and develop strategies for antimicrobial stewardship.
Acquisitions and Partnerships:
- Biotech firms acquired smaller companies with promising antimicrobial drug candidates, aiming to accelerate the development and commercialization of novel antibiotics.
- Collaborative partnerships formed between pharmaceutical companies, government agencies, and non-profit organizations to support research and development efforts in combating antimicrobial resistance.
New Product Launches:
- Pharmaceutical companies launched new antibiotics targeting multidrug-resistant pathogens, addressing unmet medical needs in critical care settings and community-acquired infections.
- Medical device manufacturers introduced innovative infection prevention technologies, such as antimicrobial coatings for catheters and surgical implants, aimed at reducing the risk of healthcare-associated infections.
Funding for Antimicrobial Research:
- Government agencies allocated funding for antimicrobial resistance research and development programs, supporting initiatives to accelerate the discovery of new antibiotics and diagnostics.
- Non-profit organizations received grants and donations to fund research projects focused on antimicrobial stewardship, infection control, and public health interventions to combat drug-resistant infections.
Global Surveillance and Reporting:
- International surveillance networks monitored antimicrobial resistance trends and provided data on resistance patterns, informing public health policies and guiding antibiotic prescribing practices.
- Collaborative efforts were made to establish standardized surveillance methods and reporting systems for antimicrobial resistance, facilitating data sharing and analysis across regions and countries.
Public Health Campaigns:
- Public health agencies launched campaigns to raise awareness about antimicrobial resistance, educate healthcare providers and the general public about prudent antibiotic use, and promote infection prevention practices.
- Educational initiatives targeted healthcare professionals, veterinarians, and agricultural workers to promote responsible antimicrobial use in human health, animal health, and agriculture sectors.
Antimicrobial Stewardship Programs:
- Healthcare facilities implemented antimicrobial stewardship programs to optimize antibiotic prescribing practices, reduce unnecessary antibiotic use, and prevent the emergence and spread of drug-resistant infections.
- Guidelines and protocols were developed for antimicrobial stewardship in various healthcare settings, including hospitals, long-term care facilities, and outpatient clinics, to ensure consistent and effective implementation.
Conclusion
Antimicrobial Resistance Statistics – Antimicrobial resistance (AMR) poses a significant global challenge, leading to increased mortality, healthcare costs, and economic burden.
Countries worldwide including Brazil, are grappling with the rise of resistant pathogens in healthcare settings.
The prevalence of resistant strains such as MRSA, ESBL-producing bacteria, and MDR-TB in Brazil highlights the urgent need for robust interventions to combat AMR.
Efforts to improve infection control practices, promote appropriate antimicrobial use, and enhance surveillance systems are crucial in mitigating the impact of AMR and safeguarding public health.
Continued collaboration and implementation of comprehensive strategies are essential to address this growing threat.
FAQs
Antimicrobial resistance refers to the ability of microorganisms, such as bacteria, viruses, fungi, and parasites, to withstand the effects of antimicrobial drugs, rendering them ineffective in treating infections.
Approximately 700,000 deaths occur worldwide each year as a result of infections caused by antimicrobial-resistant pathogens.
Antimicrobial resistance has a direct impact on the global economy. Estimates suggest that by 2050, the cumulative cost of AMR could reach $100 trillion if not effectively addressed.
Factors contributing to AMR include the misuse and overuse of antimicrobials, both in healthcare and agriculture, inadequate infection control practices, lack of access to clean water and sanitation, global travel and migration, and weak healthcare systems.
Without effective interventions, the burden of AMR is expected to increase significantly in the coming decades. Future projections include higher mortality rates, increased healthcare costs, and challenges in the research and development of new antimicrobial agents.
Discuss your needs with our analyst
Please share your requirements with more details so our analyst can check if they can solve your problem(s)



