Table of Contents
Overview
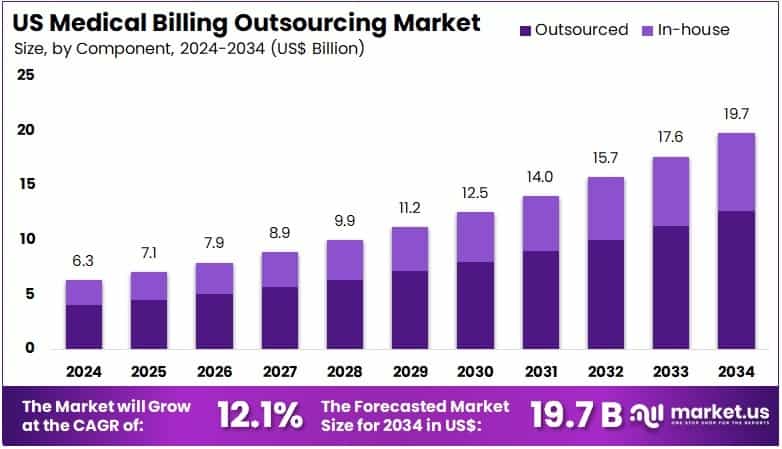
New York, NY – Aug 11, 2025: The U.S. Medical Billing Outsourcing Market is expected to grow from USD 6.3 billion in 2024 to USD 19.7 billion by 2034, expanding at a compound annual growth rate (CAGR) of 12.1%. A key factor driving this growth is the increasing administrative burden faced by healthcare providers. Managing insurance claims, coding, and paperwork requires specialized staff and often diverts attention from direct patient care. To streamline operations and focus on clinical outcomes, many hospitals, clinics, and private practices are turning to third-party billing services.
Another major driver is the growing complexity of billing regulations and compliance standards. U.S. providers must adhere to strict guidelines, including HIPAA regulations and frequently updated coding systems. Staying current requires deep expertise, which billing service providers offer. Outsourcing helps ensure accurate claims, regulatory compliance, and timely reimbursements minimizing denials and delays.
The widespread adoption of Electronic Health Records (EHRs) has also added complexity to billing. While EHRs improve access and efficiency, they must be seamlessly integrated with billing systems to avoid errors. Outsourced billing firms provide advanced tech solutions that connect smoothly with EHR platforms. Many also leverage automation and cloud-based tools, enhancing speed, accuracy, and transparency in the billing cycle.
Emerging care models such as value-based care and the rapid growth of telehealth are further transforming billing practices. These models require more detailed documentation, unique billing codes, and performance tracking challenges that outsourced providers are well-equipped to manage. Smaller and rural practices, in particular, benefit from outsourcing, as they often lack dedicated in-house billing staff. These ongoing shifts in care delivery and technology continue to fuel strong growth in the outsourcing market.
Key Takeaways
- In 2024, the U.S. medical billing outsourcing market earned US$ 6.3 billion and is projected to grow to US$ 19.7 billion by 2034.
- This market is expanding at a strong CAGR of 12.1%, reflecting increasing demand for efficient revenue cycle management in healthcare settings.
- Based on product type, front-end services led the market in 2024, capturing a dominant 47.2% share due to rising patient onboarding complexities.
- The market segments for product type also include middle-end and back-end services, but front-end operations remain most widely outsourced by providers.
- In terms of components, outsourced solutions held a commanding 63.8% market share, indicating a clear preference for third-party service providers over in-house handling.
- The in-house segment still exists but lags far behind, as healthcare organizations shift focus to clinical care rather than administrative functions.
- Among end-users, hospitals emerged as the top contributors, accounting for 58.7% of the total market revenue in medical billing outsourcing.
- Physician offices and other healthcare facilities contribute to the market, but hospitals remain the biggest adopters due to high patient volume and complex billing needs.
Segmentation Analysis
Product Type Analysis
Front-end services dominated the market in 2024 with a 47.2% share. This growth stems from the increasing need for efficient patient registration, insurance verification, and medical coding. These services help reduce claim denials and ensure accurate billing. As providers aim to enhance patient satisfaction and streamline operations, demand for front-end solutions is rising. The growing complexity of insurance rules is encouraging healthcare organizations to outsource these tasks. The adoption of digital tools and automation is further expected to accelerate the segment’s expansion.
Component Analysis
Outsourced billing services captured 63.8% of the market in 2024. Healthcare providers are turning to third-party vendors to cut operational costs and improve revenue flow. These external partners offer expertise in handling complex billing codes and navigating regulatory changes. Outsourcing also enables healthcare facilities to access advanced billing technologies without heavy investments. With a stronger focus on core healthcare delivery, organizations prefer outsourcing to ensure timely reimbursements. This shift is likely to continue as accuracy, efficiency, and compliance become more critical.
End-user Analysis
Hospitals accounted for a 58.7% revenue share in 2024, reflecting strong adoption of outsourced billing solutions. The increasing complexity of billing and regulatory requirements is driving this trend. Outsourcing helps hospitals improve efficiency, reduce administrative burden, and enhance revenue cycle performance. It also supports faster, more accurate claims processing. As hospitals face financial pressure and shift toward value-based care models, the reliance on external billing experts is expected to grow. This approach allows hospitals to prioritize clinical services while maintaining compliance and optimizing reimbursements.
Key Market Segments
By Product Type
- Front-end Services
- Middle-end Services
- Back-end Services
By Component
- In-House
- Outsourced
By End-user
- Hospitals
- Physician Offices
- Others
Key Players Analysis
Leading companies in the U.S. medical billing outsourcing market are fueling growth through mergers, acquisitions, and the adoption of cutting-edge technologies. By acquiring regional players, they expand their footprint and enhance service delivery. The use of advanced solutions, such as artificial intelligence, helps automate billing and reduce human errors. Companies are also entering underserved markets to access new customer segments. Collaborations with healthcare providers and insurers enable integrated service offerings. Maintaining compliance with evolving regulations fosters trust, ensuring sustainable growth in an increasingly competitive market.
R1 RCM Inc. stands out as a major player in the U.S. medical billing outsourcing space. It delivers end-to-end revenue cycle management services, covering patient access, medical coding, billing, and collections. Serving providers nationwide, R1 RCM has boosted its capabilities through strategic acquisitions like Acclara from Providence. This acquisition has enhanced its technology portfolio and service efficiency. With a strong focus on innovation and compliance, the company continues to deliver measurable value. R1 RCM’s operational excellence positions it as a trusted partner for healthcare organizations.
Top Key Players in the US Medical Billing Outsourcing Market
- SmarterDx
- Quest Diagnostics
- Promantra Inc
- Oracle
- McKesson Corporation
- Kyron Medical
- Kareo Inc
- eClinicalWorks
Emerging Trends
Tailored Services for Telehealth Billing
Telehealth has grown rapidly in recent years. Patients now expect virtual care to be as smooth as in-person visits. Billing for telehealth, however, is complex and requires special attention. Coding rules and insurance guidelines change often. Outsourcing firms are responding with custom solutions just for telehealth. These services help providers stay compliant and reduce claim denials. Accurate coding also leads to faster payments. Specialized billing support ensures that virtual care is properly reimbursed. As telemedicine becomes more common, demand for these tailored billing services will continue to rise.
Stronger Focus on Security and Compliance
Medical billing involves handling sensitive patient data. With more records stored digitally, data protection has become a top priority. Outsourcing firms are now investing in advanced cybersecurity tools. They also train their staff regularly on data privacy laws like HIPAA. This helps protect against breaches and maintain patient trust. Strong security also ensures compliance with industry standards. Billing partners that focus on data safety are more likely to attract long-term clients. As threats continue to evolve, maintaining strict security practices is more important than ever.
Innovation Through Blockchain and Emerging Tech
Some billing companies are exploring new technologies like blockchain. This tech adds transparency and traceability to financial transactions. It can also help reduce fraud and speed up verifications. Though still early in development, blockchain shows promise for billing. It could change how records are stored and shared. Other new tools, like machine learning, are also gaining interest. These innovations aim to improve accuracy and efficiency. Billing providers that invest in future-ready solutions stand out in a competitive market. Technology is shaping the next phase of medical billing.
Use of Global Talent to Meet Demand
The need for skilled billing professionals is growing. In response, outsourcing firms are hiring talent from around the world. This helps them maintain service quality and manage labor costs. Countries like India and the Philippines are key hubs for medical billing support. These teams work across time zones to ensure round-the-clock service. Outsourcing globally also helps fill domestic labor gaps. Trained professionals abroad bring expertise in U.S. billing rules. As workforce shortages persist, tapping into global talent allows companies to scale without compromising on performance.
Use Cases
Improving Efficiency for Hospitals and Clinics
Outsourcing medical billing helps hospitals and clinics run more smoothly. By working with expert billing firms, healthcare providers can reduce the pressure on in-house teams. These firms manage everything from coding to claims processing. This means fewer delays and fewer billing errors. Outsourcing also saves time, so staff can focus on patient care instead of paperwork. Most billing partners use digital tools to speed up the process. As a result, hospitals get paid faster and more accurately. Overall, outsourcing improves workflow, lowers overhead, and increases productivity across departments.
Support for Telemedicine Providers
Telehealth billing comes with unique challenges. It often involves different coding rules and evolving regulations. Many in-house teams struggle to keep up. Outsourcing solves this by giving providers access to experts in telehealth billing. These specialists ensure correct coding and faster claim submissions. This reduces delays and denials, which can hurt revenue. Outsourcing also helps providers stay compliant with Medicare and private payer rules. As virtual care grows, accurate billing is more important than ever. With the right partner, telemedicine practices can focus on patient care while improving reimbursement rates.
Preparing for Regulatory Changes
Healthcare rules change all the time. New billing codes, updated payer guidelines, and policy shifts can confuse internal teams. Outsourced billing providers stay updated with all changes. They adjust systems and processes quickly to remain compliant. This reduces the risk of fines or delays due to coding errors. Having an expert partner helps healthcare organizations stay ahead of audits and policy shifts. Providers can focus on patient care while billing firms manage the red tape. It’s a safer, smarter way to deal with a fast-changing healthcare system.
Enhancing Financial Visibility
Understanding revenue flow is key for healthcare growth. Many billing companies offer detailed reports and dashboards. These tools give providers clear insights into claims, collections, and denials. With this data, clinics can make better financial decisions. It also helps them plan budgets and improve cash flow. Outsourcing firms use analytics to identify trends and problems. For example, they can spot which procedures face frequent denials. With this information, providers can take action. Clear financial visibility means better planning, fewer surprises, and a stronger bottom line.
Conclusion
The U.S. medical billing outsourcing market is growing fast as healthcare providers face more complex billing rules and administrative tasks. Hospitals, clinics, and private practices are turning to third-party billing firms to improve efficiency and focus more on patient care. Outsourcing also helps them keep up with changing regulations, manage telehealth billing, and use advanced technology for better accuracy. With more use of digital tools and global talent, the industry is moving toward smarter, more secure solutions. As care models and billing systems continue to evolve, outsourcing is becoming a trusted way to boost revenue performance and reduce stress on internal teams. This trend is likely to stay strong in the years ahead.
View More
Medical Billing Outsourcing Market || Emergency Medical Services Billing Software Market || Medical Device Outsourcing Market || Medical Imaging Outsourcing Market || Healthcare Contract Research Outsourcing Market || Healthcare Supply Chain Outsourcing Market || Regulatory Affairs Outsourcing Market || Medical Affairs Outsourcing Market || Hospital Outsourcing Market || Healthcare Outsourcing Market
Discuss your needs with our analyst
Please share your requirements with more details so our analyst can check if they can solve your problem(s)



