Table of Contents
Overview
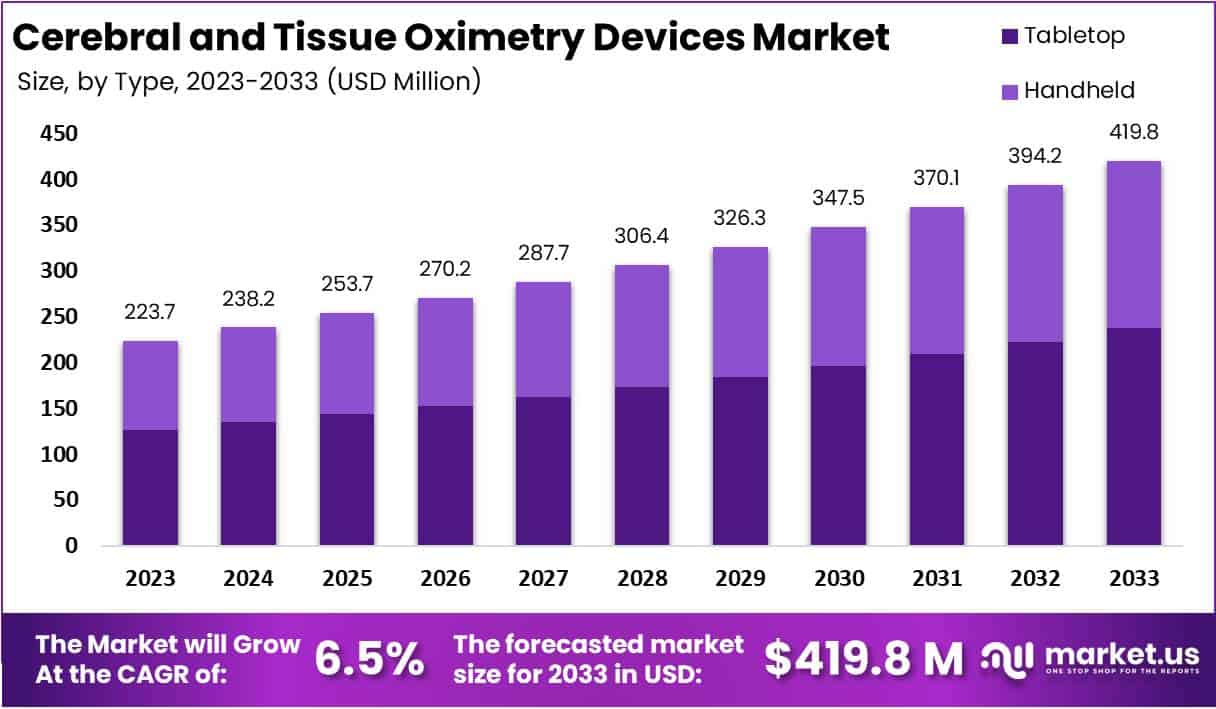
New York, NY – June 20, 2025: The Cerebral And Tissue Oximetry Devices Market is projected to grow steadily, reaching approximately USD 419.8 million by 2033. This reflects a compound annual growth rate (CAGR) of 6.5% from the 2023 value of USD 223.7 million. Several key factors are contributing to this upward trend. One major driver is the rise in surgeries requiring real-time oxygen monitoring, such as cardiac and vascular procedures. Hospitals and intensive care units are increasingly adopting these devices to prevent complications like stroke or postoperative cognitive decline. The ability to continuously track oxygen saturation in tissues ensures better outcomes and improves patient safety across critical care settings.
Technological advancement is a crucial factor shaping this market. Modern devices use multiple wavelengths in near-infrared spectroscopy (NIRS) to deliver more precise oxygen level readings. New sensors are also designed to account for variations in skin pigmentation and tissue depth. This improves accuracy across a diverse patient population. Enhanced wireless connectivity and the ability to integrate with hospital information systems have further increased the clinical appeal of these devices. As a result, healthcare providers now have access to real-time data that supports better decision-making during surgery and post-operative care.
Another strong growth factor is the global increase in elderly populations and chronic disease cases. Older adults and patients with long-term conditions are more prone to complications that require continuous tissue oxygenation monitoring. These devices are particularly useful during surgical procedures and in recovery phases. As the global burden of chronic diseases continues to rise, especially in aging populations, demand for advanced monitoring tools is growing. This trend is noticeable in both high-income and emerging countries, where healthcare systems are investing in better technologies for at-risk groups.
The expansion of home healthcare is also creating new opportunities for the market. Portable and user-friendly oximetry devices are becoming more available, allowing patients to monitor certain health conditions from home. This reduces hospital dependency and aligns with healthcare systems’ goals to improve patient management and lower overall costs. Manufacturers are now focusing on developing devices tailored for home use, which can further increase market penetration, especially among patients requiring post-surgical monitoring or chronic care management.
However, some challenges remain. High device costs, inconsistent reimbursement policies, and concerns about measurement variability in certain patient groups limit broader adoption. Smaller hospitals and clinics, particularly in low-resource regions, may find it difficult to afford these devices. Addressing these barriers through cost-effective solutions and clearer reimbursement pathways is necessary. Despite these obstacles, the market outlook remains positive, driven by technological innovation, increasing clinical use, and expanding applications in home-based care.
Key Takeaways
- The cerebral and tissue oximetry devices market is projected to reach USD 419.8 million by 2033, expanding steadily at a CAGR of 6.5%.
- Tabletop devices dominated in 2023, capturing over 56.5% market share due to advanced features and their suitability in clinical monitoring environments.
- Hospitals held the largest end-use segment in 2023, with a 52.1% share, underscoring their reliance on oximetry for patient monitoring during surgeries.
- The growing popularity of tabletop systems in 2023 was driven by smooth integration into hospital systems and enhanced real-time monitoring capabilities.
- Demand for non-invasive monitoring tools rose as healthcare providers prioritized safer, more comfortable methods for tracking patient oxygen saturation continuously.
- New technologies such as wireless connectivity and improved sensor precision have accelerated the adoption of these devices in advanced healthcare systems.
- Increasing numbers of surgeries—both in hospitals and ambulatory centers—have fueled demand for cerebral oximetry during perioperative care.
- Despite growth, high initial device costs, limited reimbursement, and occasional measurement inaccuracies remain key barriers in smaller or cost-sensitive settings.
- Significant opportunities lie in neonatal care, home healthcare, and emerging economies, along with innovation partnerships between device firms and healthcare institutions.
- North America led the global market in 2023 with a 36.5% share and USD 76.6 million revenue, supported by strong infrastructure and policy incentives.
Emerging Trends
- AI and Machine Learning Integration: Artificial intelligence and machine learning are being integrated into cerebral and tissue oximetry devices. These systems help improve the accuracy of oxygen level readings. They also adjust for factors like patient motion, skin pigmentation, and sensor positioning. Some devices now offer predictive analytics. This helps detect complications early, supporting faster medical intervention. AI also assists in reducing false alarms and improves trend analysis over time. As hospitals adopt more smart technology, AI-powered oximeters are gaining trust for use in intensive care and surgery. The integration of machine learning is making monitoring more reliable and personalized for critical care patients.
- Real-Time, Personalized Monitoring: There is a rising demand for devices that offer real-time, continuous monitoring. These systems give clinicians detailed oxygenation data every second. This helps in making quick and informed decisions, especially during surgeries or emergency care. Personalized tracking allows doctors to adjust treatment based on individual patient needs. Such features are critical in situations where brain or tissue oxygen levels change rapidly. Devices are also being designed to provide customizable alerts. These functions ensure immediate responses to abnormal readings. Real-time data not only improves safety but also supports precision medicine in both surgical and intensive care environments.
- Portable and Wearable Designs: Wearable oximetry devices are becoming more common in healthcare. They are especially useful for patients with chronic illnesses such as COPD or those recovering after surgery. These new devices are small, light, and comfortable for daily use. Some models use fiber-free or in-ear sensors, making them less intrusive. Wearables allow patients to monitor oxygen levels outside hospitals. This helps reduce hospital stays and supports better home care. Clinicians can also access patient data remotely. As telehealth grows, the demand for wearable monitoring systems continues to rise. These devices help extend care into everyday life.
- Advancements in Sensor Technology: Sensor technology in oximeters is advancing quickly. Many devices now use multi-wavelength near-infrared spectroscopy (NIRS). This technology improves tissue penetration and gives more accurate readings. Modular sensor designs also offer flexibility. They can be adjusted for different body sites or clinical needs. New sensors work better across different skin types and tissue densities. They also reduce interference from external light or movement. These upgrades ensure consistent and dependable results. Improved sensor precision is critical for patients in intensive care, surgery, and neonatal units. Hospitals now prefer devices that combine deep tissue sensing with user-friendly setup.
- Wireless Connectivity and Telehealth Integration: Modern oximetry devices now include wireless data transfer. This supports seamless integration with hospital systems and telemedicine platforms. Remote access to patient data helps clinicians monitor conditions from anywhere. This is especially useful for home care and outpatient management. Devices that store and transmit data wirelessly save time and improve accuracy. Many systems now sync with smartphones or cloud platforms. This allows for better tracking and communication between patients and providers. As virtual care expands, connectivity is becoming a standard feature in oximetry devices. It ensures timely interventions and improves patient engagement.
- Shift Toward Non-Invasive Monitoring: The market is shifting from invasive to non-invasive monitoring methods. Non-invasive oximetry offers better comfort and safety for patients. It reduces infection risks and eliminates the need for catheter-based systems. Devices now use surface sensors to monitor oxygen levels without puncturing the skin. This approach is suitable for both short-term and long-term use. Non-invasive monitoring is gaining popularity in neonatal care, emergency medicine, and outpatient surgery. It is also preferred in home settings. As patients and clinicians demand safer and easier tools, non-invasive technologies are becoming the standard across healthcare facilities.
- Modular and Specialty-Focused Design: Device manufacturers are now offering modular systems tailored for specific medical fields. For example, neurosurgery, neonatal care, and cardiac surgery benefit from specialized monitoring solutions. Modular oximeters allow clinicians to add or remove features based on the clinical need. This flexibility helps hospitals use one system across various departments. Some devices also offer multi-site monitoring, allowing clinicians to assess oxygenation in different body regions simultaneously. Customization improves usability and patient outcomes. These tailored systems are being widely adopted in advanced surgical centers and intensive care units. The trend reflects the growing need for targeted, adaptable solutions.
- Expanding into Neonatal and Home Care: Cerebral and tissue oximetry is increasingly used in neonatal care. Preterm infants need constant monitoring of brain oxygen levels. These devices support early detection of hypoxia and help prevent long-term complications. Lightweight sensors designed for small patients are gaining adoption in neonatal intensive care units (NICUs). In addition, oximeters are expanding into home healthcare. Chronic care patients can now track oxygenation at home with portable devices. This reduces hospital visits and improves long-term care. The expansion into home and neonatal care highlights the market’s shift toward continuous, preventive monitoring in both clinical and non-clinical settings.
Use Cases
- Neurosurgery and ICU Monitoring: Cerebral oximetry is widely used in neurosurgery and intensive care units. It allows for continuous monitoring of cerebral tissue oxygen saturation (SctO₂) using near-infrared sensors. This is crucial during critical neurological events. For instance, in patients diagnosed with brain death, SctO₂ levels have been shown to drop from approximately 71% to 54% within just 1 to 3 hours. This rapid decline highlights the value of real-time monitoring in early diagnosis and intervention. The technology supports medical teams in avoiding delayed responses to neurological deterioration and helps improve patient outcomes in both ICU and surgical environments.
- Heart Surgery and Perioperative Care: Cerebral oximeters are increasingly used during heart surgeries, especially in procedures involving cardiopulmonary bypass. These devices help guide brain perfusion and ensure oxygen delivery during operations. Their use has been linked to improved postoperative recovery. A meta-analysis found that adult patients monitored with cerebral oximetry had a lower risk of developing postoperative cognitive dysfunction (POCD). This shows the technology’s role in protecting neurological function during and after surgery. It also supports better perfusion management, reducing complications and enhancing surgical safety. The devices are now standard in many cardiac surgery protocols worldwide.
- Neonatal and Pediatric Care: Cerebral and tissue oximeters are essential in neonatal intensive care units (NICUs), particularly for preterm infants. These babies are at risk of cerebral hypoxia due to underdeveloped organs. Oximetry enables real-time monitoring of brain oxygen levels at the bedside. This helps clinicians make immediate decisions to prevent brain damage. In many cases, early detection of low oxygen saturation leads to faster interventions and improved neurological development. The technology supports clinicians in stabilizing the infant’s condition, enhancing survival rates and long-term outcomes. Its non-invasive nature makes it highly suitable for continuous monitoring in vulnerable newborns.
- Resuscitation and Post-Cardiac Arrest Monitoring: Cerebral oximetry is also used during emergency resuscitation and recovery after cardiac arrest. For example, in cesarean section (C-section) cases requiring resuscitation, monitoring ScO₂ levels helps detect hypoxia at an early stage. This allows clinicians to respond quickly and potentially reduce the length of ICU stays. Maintaining optimal ScO₂ levels after cardiac events is linked with improved neurological outcomes. By offering continuous oxygenation data, the device supports targeted therapy and better prognostic evaluation. The approach is gaining popularity in emergency care protocols and is being studied for its ability to reduce long-term cognitive impairment.
- Remote and Wearable Brain Monitoring: Wearable cerebral oximeters are becoming more accurate and user-friendly. In-ear devices now offer about 94% accuracy in classifying cognitive states. These readings are also 12 seconds faster than traditional finger-based sensors. Another breakthrough is the fiber-free phase-modulated diffuse speckle contrast flow (PM-DSCF) device. It achieves deeper tissue penetration—up to 17.5 mm compared to 7.5 mm in earlier models. These advances support continuous cerebral blood flow monitoring outside hospital settings. They are particularly useful for home care, rehabilitation, and outpatient neurology. The portability of these devices is helping to expand their use across new care models.
- Sports, Cognitive Load, and Brain Research: Cerebral oximetry devices are increasingly used in sports science, cognitive workload monitoring, and brain–computer interface (BCI) research. In neuroergonomics, the technology detects cerebral blood flow changes of around 8% to 12% during mental tasks. This helps researchers assess cognitive load and brain performance in real-time. Applications include virtual reality simulations, cognitive fatigue studies, and BCI training. The insights gained from this monitoring are useful in designing safer work environments and improving mental task efficiency. It also enables precise assessment of how individuals respond to stress, exercise, and workload, especially in high-performance and clinical settings.
Conclusion
In conclusion, the cerebral and tissue oximetry devices market is growing steadily due to rising use in surgeries, intensive care, and neonatal monitoring. These devices are valued for their non-invasive design, real-time data, and ability to support better patient outcomes. Technological advancements such as wireless features, smart sensors, and wearable designs are increasing their use in both hospitals and home care. Although high costs and limited access in low-resource settings remain challenges, ongoing innovation and expanding applications are driving adoption. As healthcare shifts toward continuous and personalized monitoring, cerebral oximetry is becoming a key tool for safer, smarter patient care across various medical fields.
Discuss your needs with our analyst
Please share your requirements with more details so our analyst can check if they can solve your problem(s)



