Table of Contents
Overview
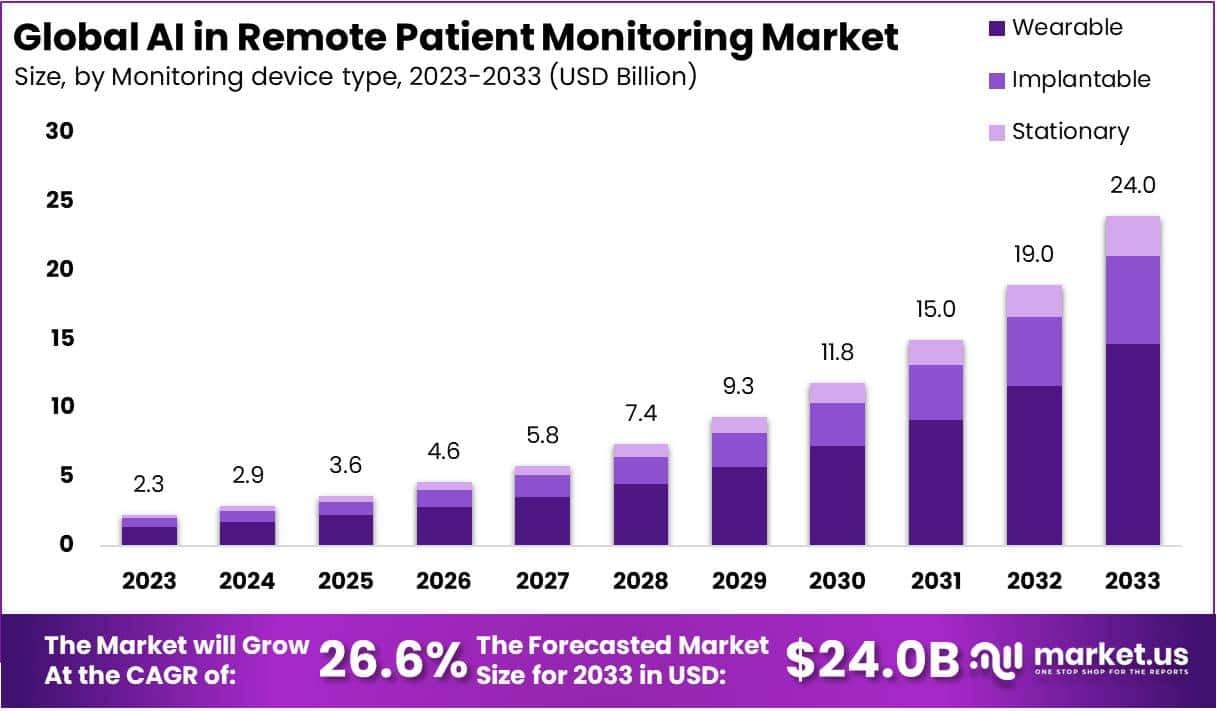
The global AI in remote patient monitoring market is projected to reach nearly USD 24 billion by 2033 from USD 2.3 billion in 2023, growing at a CAGR of 26.6%. Growth is driven by rising demand for continuous healthcare delivery beyond clinical settings, increased chronic disease cases, and initiatives favoring telehealth adoption. The shift toward value-based healthcare has strengthened the relevance of AI-powered monitoring solutions. As healthcare systems emphasize cost efficiency and improved patient outcomes, the adoption of AI-enabled tools is expected to rise steadily.
Technological developments have played a critical role in market expansion. Advancements in artificial intelligence, machine learning, and edge computing have improved predictive analytics and automated clinical decision support. Enhanced sensor accuracy and smart wearable devices enable continuous health data collection and analysis. These innovations allow real-time monitoring and early risk detection, supporting timely medical intervention. As integration capabilities with electronic health records improve, providers are increasingly confident in deploying AI-driven remote care systems.
Chronic diseases such as diabetes, cardiovascular conditions, and respiratory disorders have increased globally, contributing significantly to healthcare spending. AI-supported remote monitoring facilitates early diagnosis and proactive disease management, which reduces hospital readmissions and enhances patient quality of life. Continuous monitoring capabilities are particularly valuable for aging populations and patients requiring long-term supervision. As healthcare delivery moves toward prevention and personalized care, AI-based monitoring systems are positioned to support disease management more effectively.
The demand for home-based care has risen considerably, influenced by patient preference and the post-pandemic digital health momentum. AI-enabled RPM platforms support remote consultations and treatment, reducing the strain on hospitals and improving access in rural or underserved regions. Favorable reimbursement frameworks and government support for digital health technologies have provided a solid regulatory foundation. Clearer pathways for AI-driven medical device approval are expected to further stimulate investment and adoption.
Cost efficiency and workforce optimization remain key market drivers. AI systems assist clinicians by automating routine tasks, triaging patients, and reviewing large medical datasets, helping address staff shortages and reduce operational burden. Partnerships between healthcare providers, technology firms, and investors have accelerated innovation and commercial deployment. As remote monitoring becomes embedded in patient-care pathways, continued investment, improved interoperability, and demand for predictive healthcare services are anticipated to drive long-term market growth.
Key Takeaways
- The wearable monitoring device segment held a dominant position in 2023, surpassing AI-based tools as healthcare providers favored continuous patient insights through advanced wearable solutions.
- Software solutions accounted for approximately 75.3% market share due to increasing adoption for accurate diagnostics, enhanced treatment decision-making, and improved remote patient care workflows.
- Machine learning technology secured a leading share in 2023, supported by its expanding role in predictive analytics, patient outcome optimization, and real-time healthcare data processing.
- Chronic disease management applications remained the primary growth driver, fueled by rising long-term illness cases and preference for AI-enabled monitoring in treatment continuity.
- Market expansion was significantly supported by increasing chronic illness prevalence and the cost-efficiency advantages of AI-powered remote patient monitoring systems across diverse healthcare settings.
- Growth momentum was hindered by limited awareness of AI-based remote monitoring solutions and inadequate healthcare infrastructure in underserved regions, restricting adoption potential.
Regional Analysis
North America was observed to lead the AI-driven remote patient monitoring market. In 2023, the region accounted for 29.9% share, reflecting strong technological capabilities. Growth was attributed to the presence of established healthcare infrastructures and major market participants. Adoption of advanced medical technologies remained high in the United States and Canada. Rising healthcare expenditure further supported market progress. Continuous investment in digital health initiatives strengthened industry expansion. Demand for innovative patient monitoring systems increased. These aspects collectively contributed to the region’s dominant market position during the assessment year.
Chronic disease prevalence further accelerated market growth. A substantial portion of the population faced long-term medical conditions requiring continuous care. According to the Centers for Disease Control and Prevention, heart disease affected more than 79 million individuals in the United States and accounted for approximately 40% of deaths. Moreover, projections indicated that nearly 133 million Americans, or half of the population, lived with at least one chronic condition, including heart disease, arthritis, and hypertension. Demand for AI-enabled monitoring thus increased significantly.
Digital readiness played a major role in market expansion. North America demonstrated high adoption of smartphones, internet services, and social media platforms. Improved broadband connectivity supported seamless real-time health data transmission. Patients increasingly preferred home-based monitoring and virtual medical interactions. Healthcare systems reduced dependence on in-person visits. AI solutions enabled proactive disease management. Remote care delivery gained substantial traction. Widespread use of wearable devices and smart health applications fostered increased dependence on digital healthcare tools. This led to strong integration of AI in monitoring technologies across the region.
Regulatory compliance strengthened industry development. The region maintained strict standards for AI-based healthcare tools, supporting patient safety and technology reliability. Favorable reimbursement systems further encouraged utilization of remote monitoring solutions. Providers adopted AI systems to improve efficiency and reduce hospitalization rates. Government programs emphasized value-based care, enhancing remote patient services. As digital transformation continued, sustained investment in AI-driven healthcare platforms was projected. North America was expected to maintain its leading position due to technological maturity and strong policy frameworks.
Segmentation Analysis
The wearable device segment held the dominant position in AI-enabled remote patient monitoring in 2023. It accounted for 61.2% of total revenue. Growth was driven by wearable devices that track indicators such as heart rate, blood pressure, glucose, and oxygen saturation. These tools enable continuous health assessment and early intervention. Wearables detect subtle physiological changes and alert care teams. Recent innovations, such as Fitbit Sense 2 and Versa 2, strengthened adoption. As a result, the segment remained essential for advancing home-based patient monitoring.
AI-driven software solutions were most essential within the component category in 2023. Software captured approximately 75.3% market share. Demand increased due to the need for advanced AI tools capable of handling large patient datasets and automating clinical workflows. Clinicians used these platforms to monitor patients remotely and maintain care quality, especially during the COVID-19 period. Philips’ IntelliSpace Corsium supported chronic care management and decision-making. As adoption rises, software remains vital for enhancing RPM efficiency and care delivery.
Machine learning technologies led the technology landscape in AI remote monitoring in 2023. This segment secured a 53.9% market share. The dominance was attributed to machine learning’s ability to process extensive datasets from wearables and medical sensors. Predictive analytics enabled healthcare providers to identify risks, detect anomalies, and guide timely interventions. Machine learning models recognized deviations from baseline health patterns. As data volumes grow, the segment is expected to advance predictive care models and streamline real-time patient evaluation across healthcare systems.
Chronic disease management remained a core application area in 2023. This segment held a 55.2% share as chronic illness cases increased globally. AI-enabled remote monitoring supported continuous assessment of conditions such as diabetes, cardiovascular disorders, and hypertension. Clinicians tracked symptoms and medication adherence to improve outcomes. According to the International Diabetes Federation, diabetes cases are forecast to rise to 6.48 billion by 2030. AI platforms enabled better long-term management, thus reinforcing dominance of chronic disease monitoring across healthcare markets.
Key Market Segments
By Monitoring Device Type
- Wearable
- Implantable
- Stationary
By Component
- Hardware
- Software
- Services
By Technology
- Machine Learning
- Natural Language Processing
- Computer Vision
- Others
By Application
- Chronic Disease Management
- Geriatric Care Management
- Sleep Apnea Monitoring
- Fitness Monitoring
- Other
Key Players Analysis
Innovation in artificial intelligence and digital health solutions is driving competitive activity in remote patient monitoring. Market participants are increasing investment in research and development to create advanced platforms that enhance diagnosis, automate clinical workflows, and improve patient outcomes. Their focus is on scalable, secure, and data-driven systems that support chronic disease management and predictive care pathways. Companies such as BPG Bio, Inc., Ferrum Health, and Caption Health Inc. are emphasizing algorithm accuracy, early detection capabilities, and medical-grade compliance to strengthen their global footprint.
Strategic partnerships are widely adopted to accelerate technology capabilities and expand service offerings. Market entrants and established vendors are collaborating with healthcare providers, insurers, and technology partners to broaden deployment and integration levels. These alliances support interoperability, improve care coordination, and advance smart monitoring functions. Sensely Inc., AICure LLC, and Medasense Biometrics Ltd are pursuing collaboration models that align with virtual care adoption, patient engagement needs, and AI-based clinical analytics.
Corporate expansion strategies are increasingly focused on mergers and acquisitions to secure technological assets and commercial infrastructure. Companies aim to strengthen product pipelines, expand geographically, and enhance AI modeling capabilities for real-time patient assessment. Nuance Communications and Atomwise Inc. have demonstrated acquisition-driven approaches to boost development resources, enrich clinical datasets, and improve computational accuracy. These moves enable faster product delivery, deeper integration with health platforms, and higher competitive advantage within the remote monitoring landscape.
Product innovations remain central to maintaining market leadership and capturing emerging opportunities. Leading firms are launching advanced AI-enabled remote monitoring platforms that support continuous data evaluation, anomaly detection, and clinician decision support. International Business Machines Corp. and Modernizing Medicine, Inc. are investing in scalable cloud-based ecosystems and machine-learning architectures that deliver personalized care insights. Such technology is improving clinician efficiency, enabling preventative interventions, and supporting outcome-driven healthcare delivery across varied medical settings and patient populations.
Challenges
1. Data quality and real-world model performance
Remote monitoring devices in homes and daily life often face motion, poor usage, and signal errors. These issues reduce data quality and weaken model accuracy. Outside controlled trials, model drift can occur, leading to unreliable predictions or delayed alerts. Research highlights challenges with PPG sensors and similar technologies, showing that noise and artifacts remain common. As a result, strong AI techniques are required to clean signals and adjust for real-world variation. Continuous calibration and feedback loops are essential. Ongoing performance checks help maintain reliability and encourage adoption in clinical environments.
2. Bias, fairness, and health equity
AI systems trained on narrow or non-diverse datasets may perform poorly for underrepresented groups. This can lead to unequal care, missed diagnoses, and widening health gaps. Academic reviews note that bias in healthcare AI remains a serious concern. Clear testing across demographic groups is needed to ensure fairness. Transparent reporting, bias audits, and diverse data sources support equitable results. Providers must evaluate models before deployment to prevent unintended harm. Ethical design and community engagement can improve outcomes. Continuous monitoring is required as models are updated and used across new populations.
3. Cybersecurity and privacy risks
Connected sensors and platforms increase exposure to cyber threats. Weak device security can put health data at risk. Breaches may reveal personal medical information or allow unauthorized access to devices. Regulatory bodies outline cybersecurity expectations for medical tools, and advisories regularly warn about vulnerabilities. Vendors must follow secure-by-design practices, use encryption, and update devices regularly. Providers also play a role by enforcing strong access policies. Routine testing and rapid response plans reduce risk. Patient trust depends on robust safeguards and ongoing vigilance against evolving cyber threats.
4. Clinical validation and evidence standards
Many AI tools in remote care lack strong clinical trials across diverse settings. Evidence exists but can vary widely in study design, outcomes, and follow-up periods. This variability makes it difficult for clinicians and insurers to fully trust results. Randomized and real-world studies are needed to support responsible adoption. Standard measures and transparent reporting improve clarity. Wider validation helps models perform reliably across populations and care environments. Better evidence also aids payer approval and reimbursement decisions. As standards grow, vendors must invest in rigorous clinical testing.
5. Regulatory and change-management complexity
AI technologies evolve over time, which creates regulatory challenges. Compliance requires detailed documentation, clear labeling, and strong scientific reasoning for updates. Post-market monitoring and defined update plans support ongoing safety. These steps add time and effort for developers and providers. Structured processes help maintain trust and limit risk. Regulatory frameworks continue to evolve, and organizations must stay informed. Effective governance ensures models remain safe and consistent as technology advances. Change-management practices also help clinicians adopt new systems smoothly.
6. Interoperability and workflow integration
Remote patient data must connect smoothly to clinical systems. If information does not flow into electronic health records or support everyday decisions, clinicians struggle to act on alerts. Poor integration can lead to alert fatigue and workflow stress. Guidance outlines interoperability needs, yet adoption remains uneven. Standardized data formats and seamless interfaces help improve efficiency. Effective systems present insights clearly and reduce manual work. Successful integration supports better care and improves clinician confidence in AI tools.
7. Reimbursement clarity and sustainability
Remote patient monitoring receives support in public programs, including Medicare. However, reimbursement rules continue to evolve. Coding, billing processes, and payment levels are updated frequently. Policy shifts affect providers and clinics, including rural and community health centers. Organizations must follow changes closely to maintain compliance and financial stability. Clear reimbursement pathways encourage adoption and long-term use. Sustainable payment models ensure remote care remains accessible and scalable. Future policies may expand coverage, but ongoing attention is necessary.
8. Digital literacy and patient adherence
Patients must understand how to use devices and applications correctly. Usability challenges can limit data quality and engagement. Survey results show that digital readiness varies across ages, regions, and socioeconomic levels. Some patients face difficulty with technology setup or daily device use. Simple interfaces, user support, and education improve participation. Tools designed with accessibility in mind help broaden engagement. Providers should address barriers early and offer guidance to build confidence. Strong patient support increases adherence and long-term effectiveness of remote monitoring programs.
Opportunities
1. Earlier detection and proactive care
Remote patient monitoring uses continuous data to detect health issues sooner. Subtle changes in vital signs or symptoms can signal early deterioration, such as heart failure worsening. Predictive models and machine-learning tools support this process by identifying risk patterns in real time. Earlier alerts allow providers to intervene before complications develop, which reduces avoidable hospital visits and emergency use. Multiple studies and clinical programs have shown meaningful reductions in acute-care utilization. This improvement supports better outcomes and helps health systems move toward proactive, preventive care rather than reactive treatment.
2. Scalable chronic-disease management
Chronic diseases place consistent pressure on healthcare systems. Remote monitoring enables structured and repeatable care processes for conditions such as hypertension, diabetes, COPD, and heart failure. Clear pathways and workflow standards have been adopted in primary care and specialist settings across the United States. Regular data review, automated reminders, and coordinated communication between clinicians and patients help maintain disease control. This model scales without requiring constant in-person visits. As a result, more patients can be managed efficiently, and adherence to treatment plans improves. Better long-term management supports lower costs and stronger population-health outcomes.
3. Better access and equity for remote populations
Remote monitoring connects patients in underserved and rural regions with specialists and timely clinical support. It reduces travel barriers and long wait times, which often limit care in remote areas. Telehealth infrastructure combined with monitoring devices ensures consistent communication and oversight. International public-health guidance, including insights from the World Health Organization, emphasizes equity and digital access. Countries are adopting programs to bridge gaps in rural healthcare delivery. By extending high-quality care beyond traditional facilities, remote patient monitoring enhances inclusion, improves chronic-disease control, and promotes health equity for populations that historically face care disparities.
4. Outcomes and cost signals
Evidence from meta-analyses and real-world studies shows that remote monitoring is linked to lower hospital admissions and shorter inpatient stays. Better symptom tracking and timely interventions help prevent complications that would otherwise require emergency treatment. These clinical improvements align with value-based care models that reward efficiency and strong patient outcomes. Payers and providers are increasingly focused on programs that reduce unnecessary utilization. As adoption expands, further data is expected to reinforce cost savings and care-quality gains. This pattern supports continued investment in remote monitoring technologies and programs across integrated health systems.
5. Regulatory momentum for AI in devices
AI-driven healthcare devices and software are gaining regulatory clarity. The U.S. Food and Drug Administration has introduced guidance specific to AI and machine-learning systems in medical devices. Key elements include lifecycle oversight and predetermined change-control plans that guide safe model updates. These frameworks allow companies to refine algorithms responsibly and maintain high safety standards. As compliance expectations become more explicit, developers of remote monitoring solutions can innovate with greater confidence. This direction supports more adaptive AI tools, enabling continuous improvement and more accurate patient-risk insights in clinical environments.
6. Workforce augmentation
Remote monitoring generates large volumes of patient data. AI-based triage and summarization tools help clinicians manage this information by highlighting key risks and filtering routine data. This reduces administrative burden and directs attention to patients who need immediate support. Best-practice guidance in telehealth emphasizes structured workflows, ongoing engagement, and clear escalation paths. Automation assists staff, strengthens efficiency, and supports consistent quality. As staffing shortages continue in many health systems, AI-enabled monitoring tools can help clinicians manage larger patient panels while maintaining safe and effective care delivery.
Conclusion
The market for AI in remote patient monitoring is expected to grow steadily due to rising demand for continuous care outside hospitals. Adoption is supported by strong movement toward value-based healthcare, higher chronic illness cases, and a clear shift to home-based services. Advances in smart wearables, predictive analytics, and automated decision support have strengthened real-time care and early intervention. Favorable digital health policies and wider use of connected devices are expected to encourage more healthcare providers to use AI-enabled platforms. As digital transformation expands, sustained investment, better data integration, and stronger clinical confidence are anticipated to support long-term growth in this industry.
Discuss your needs with our analyst
Please share your requirements with more details so our analyst can check if they can solve your problem(s)



